
ii
Suggested citation: European Centre for Disease Prevention and Control and European Union Aviation Safety Agency.
Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol.
2 December 2020. ECDC: Stockholm; 2020/EASA: Cologne; 2020.
© European Centre for Disease Prevention and Control/European Union Aviation Safety Agency 2020
Reproduction is authorised, provided the source is acknowledged.

ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
1
Contents
Definitions ...................................................................................................................................... 2
Executive summary ......................................................................................................................... 3
1. Context ....................................................................................................................................... 4
2. Risk assessment and scientific evidence ........................................................................................ 5
2.1 Travel-related risks in the COVID-19 pandemic ..............................................................................5
2.2 Testing and quarantine measures for air travel ..............................................................................7
2.2.1 Testing of air travellers .......................................................................................................... 7
2.2.2 Quarantine of air travellers ..................................................................................................10
2.2.3 Combination of testing and quarantine for air travellers .....................................................10
3. Operational recommendations .................................................................................................... 11
References .................................................................................................................................... 14
Annex 1. Overview of travel-related measures (air travel) with advantages and disadvantages .......... 17
Annex 2. Guidelines for travel-related measures air travel
7
............................................................ 19
Annex 3. Overview of quarantine, testing combinations and effectiveness in preventing local transmission .... 20

ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
2
Definitions
Asymptomatic: refers to people who are infected but do not exhibit symptoms of COVID-19.
Contacts of confirmed cases: refers to any person who has had exposure to a confirmed COVID-19 case
within a timeframe ranging from two days before to 10 days after the onset of symptoms. If the case has had
no symptoms, further assessment should be made, as outlined in ‘Contact tracing: public health management
of persons, including healthcare workers, who have had contact with COVID-19 cases in the European Union
– third update’ [1].
COVID-19: refers to corona virus disease 2019 – a potentially severe illness caused by a SARS-CoV-2 most
frequently characterised by fever, coughing, and shortness of breath. Other organs may be affected, resulting
in specific symptomatology.
Epidemiology: refers to the branch of medicine that deals with the study of the incidence, distribution and
determinants of disease and the analysis of these measures in order to control the spread of diseases and
improve other factors related to health.
False negative: refers to a test result indicating that the disease is not present when the person actually does
have the disease.
False positive: refers to a test result indicating that the disease is present when the person actually does not
have the disease.
IHR: international health regulations, refers to an overarching legal framework that defines countries’ rights
and obligations in handling public health events and emergencies that have the potential to cross borders.
Incidence: refers to the number of new cases of a disease over occurrence, rate or frequency of a disease - in
this context the number of new cases during a specified period.
Positive predictive value (PPV): refers to the likelihood of a positive test being true positive.
PoE: Point of Entry
Prevalence: the proportion of the population with a disease at a specific point or period in relation to disease
burden expressed as a percentage or rate with the total population as the denominator.
RADT: rapid antigen detection test, is a testing method for SARS-CoV-2 that can rapidly (usually in <30
minutes) detect viral components present during the infection in samples such as nasopharyngeal secretions.
RT-PCR: reverse transcription polymerase reaction - a very sensitive testing method for detecting different
pathogens based on their genetic material. It is considered to be the gold standard for the detection of SARS-
CoV-2 RNA.
Non-symptomatic: refers to persons who may or may not be infected and do not exhibit COVID-19
symptoms.
Negative predictive value (NPV): refers to the likelihood of a negative test being true negative.
Quarantine of contacts of cases: refers to the need for those exposed to a confirmed COVID-19 case to
remain at home or in a designated safe setting for a defined period after the last exposure, with the aim of
reducing virus transmission [1]. This can be voluntary, or mandatory, if implemented by local authorities.
Quarantine of travellers: refers to travellers being required to remain at home or in a designated safe setting
for a defined period after entering a region or country. This can be voluntary or mandatory, if implemented
by local authorities.
SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2, the causative agent of COVID-19.

ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
3
Executive summary
This document aims to support Member States in determining a coordinated approach to reduce the risks related
to the movement of people within and between the EU/EEA countries and the UK in the context of the COVID-19
pandemic. It is intended for use by decision-makers in the Member States, including public health authorities and
civil aviation authorities, as well as aviation stakeholders. The recommendations outlined in this document may
also be taken into account by Member States when considering temporary restrictions on non-essential travel to
the EU in relation to residents of third countries
1
.
The document provides information on effective and differentiated strategies to enable the health authorities to
evaluate scenarios and make informed decisions on the best possible measures.
Scientific evidence and information, presented and analysed in this document, give rise to the following key
considerations:
In the current epidemiological situation, where SARS-CoV-2 is established in all EU/EEA countries and the UK,
imported cases account for a very small proportion of all detected cases and are unlikely to significantly
increase the rate of transmission.
The prevalence of SARS-CoV-2 in travellers is estimated likely to be lower than the prevalence in the general
population or among contacts of confirmed cases.
Travellers should not be considered as a high-risk population, nor treated as contacts of COVID-19 cases,
unless they had been in known contact with a confirmed positive case.
Travellers should be subject to the same regulations or recommendations as applied to the local population.
Member States should always admit their own nationals and EU citizens and their family members resident in
their territory, and should facilitate swift transit through their territories.
Decision makers are invited to consider the detailed epidemiological evidence that supports the options presented
in this document acknowledging that:
In the current epidemiological situation
2
, quarantine or systematic testing for SARS-CoV-2 of air travellers is
not recommended.
Harmonisation among Member States is recommended based on the specific measures presented in this
document.
Chapter 3 outlines the main risk assessment criteria and the available evidence and information on the use of
testing and quarantine for travellers. Where scientific evidence is insufficient, the document takes into
consideration modelling studies and expert opinions from the relevant experts at the European Centre for Disease
Prevention and Control (ECDC) and the European Union Aviation Safety Agency (EASA).
In Chapter 4, the document presents specific operational recommendations for the management of these travel-
related measures by the Member States.
The document, its observations, recommendations and conclusions are based on the evidence and best knowledge
available at the time of writing, as compiled and analysed by experts at ECDC and EASA. Depending on the
evolution of the pandemic and future evidence and developments, in terms of risk assessment criteria, testing
technologies or the introduction of vaccines, this document may require updating which may prompt further
assessment by the Member States in their implementation efforts.
1
In accordance with Council Recommendation (EU) 2020/912 of 30 June 2020 on the temporary restriction on non-essential
travel into the EU and the possible lifting of such restriction; OJ L 208I 1.7.2020, p.1. Available at: https://eur-
lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A02020H0912-20201026&qid=1606575297003
2
At the time of writing, community transmission is occurring in all EU/EEA Member States and the UK.

ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
4
1. Context
Within the EU/EEA and the UK, cross-border travel can refer to travel within the EU/EEA and the UK and travel
from third countries outside the EU/EEA and the UK. Travellers within the EU/EEA and the UK include not only
tourists, but also transport workers, commuters, students, military and diplomatic personnel, business travellers
and seasonal workers. Free movement within the EU is one of the fundamental principles of the Treaty on the
Functioning of the European Union [2].
In response to the first wave of COVID-19 in spring 2020, the EU/EEA countries and the UK implemented various
public health measures to minimise the likelihood of COVID-19 transmission on-board various conveyances
including aircraft, as well as other measures to limit the importation of COVID-19 by cross-border travel. To
support the Member States, EASA and ECDC jointly developed the COVID-19 Aviation Health Safety Protocol
(AHSP) [3], which provides recommendations on measures for every stage of the end-to-end traveller journey [3].
The COVID-19 AHSP also provides recommendations regarding pre- and post-flight health screening and
supportive arguments for the collection and sharing of passenger locator data.
The travel-related measures adopted by the EU/EEA countries and the UK in the context of the COVID-19
pandemic have varied significantly and some of them have had an impact on citizens’ rights to free movement and
the functioning of the internal market. Most of the EU/EEA countries and the UK have developed national criteria to
determine the potential need for testing and/or voluntary or mandatory quarantine of incoming travellers. Due to
the rapidly-evolving epidemiological situation the measures have changed on average every 714 days. Despite
initiatives such as the European Commission’s Re-Open EU website [4] and the EU health preparedness
recommendations for a common EU testing approach to COVID-19, agreed by the Health Security Committee
(HSC) [5], the different measures have resulted in significant confusion for travellers. This is continuing to have a
significant negative impact on travel and tourism.
On 13 October 2020, the Council of the European Union adopted Recommendation 2020/1475 on a coordinated
approach to the restriction of free movement in response to the COVID-19 pandemic, aiming to avoid
fragmentation and disruption, and to increase harmonisation, transparency and predictability for citizens and
businesses [6].
On 28 October 2020, the European Commission issued a Communication on additional COVID-19 response
measures [7], mandating EASA and ECDC to work on guidelines on testing in air travel which could be used by
public health authorities, airlines and airports to help the safe arrival of passengers, along with a Commission
Recommendation on COVID-19 testing strategies, including the use of rapid antigen tests [8].
ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
5
2. Risk assessment and scientific evidence
2.1 Travel-related risks in the COVID-19 pandemic
Travel and population movements contribute to the spread of pathogens and/or their introduction into areas where
they were not previously circulating [9]. Historically, governments intuitively turn to travel-related measures and
restrictions, which potentially help build public trust, particularly for new emerging threats to health [10]. Advice
against non-essential travel during an epidemic is designed to reduce the number of people who may be exposed
while visiting areas or countries where community transmission is ongoing and, consequently, to reduce the risk of
importation and transmission among travellers during transportation.
The first cases of COVID-19 in Europe were imported from Hubei, China. However, it is difficult to identify the first
actual importation and it is postulated that the pathogen was silently circulating for weeks before its detection.
Travel-related virus introduction and tourism-related spread within the EU/EEA and the UK contributed
substantially to the transmission across and within countries during the early phase of the COVID-19 pandemic
[11-17].
Moreover, models consistently indicate that neither temperature screening, nor surveillance of passengers at
airports to identify those exhibiting COVID-19 relevant symptoms would have a major impact on the detection of
imported COVID-19 cases [18,19]. A modelling study (in preprint) estimates that imported COVID-19 cases, using
the May 2019 travel volumes, would have accounted for less than 1% of the total of cases in 48 countries and less
than 10% in 142 countries around the world in May 2020 [20]. Therefore, in most countries, imported cases are
likely to contribute little to the ongoing spread of SARS-CoV-2, once the virus has been introduced in the
community.
With an effective reproduction number of COVID-19 between 24 (high) [21] and a long incubation period (114
days; median 57 days) [22], models estimated that a 90% reduction of the number of passengers would only
delay the arrival of the outbreak in a country by approximately 10 days [23].
Based on evidence from past outbreaks of new emerging pathogens, as well as the above mentioned models
[10,24,25], it is assessed that entry screening for COVID-19, quarantine and border closure for incoming travellers
are unlikely to prevent the introduction of SARS-CoV-2 in a community but may delay it for a short period of time.
However, public health capacity should be in place to promptly recognise new cases through comprehensive
surveillance; undertake prompt testing and isolation of cases and carry out contact tracing for incoming travellers
and quarantining of exposed contacts.
As regards air travel, documented cases of SARS-CoV-2 transmission in aircraft mainly occurred before the
implementation of non-pharmaceutical interventions (NPI) [26,27]. To minimise the risk of transmission of SARS-
CoV-2 during air travel, EASA and ECDC developed a dedicated COVID-19 Aviation Health Safety Protocol (AHSP)
addressing all stages of travel and describing all the measures including communication, administrative controls,
physical distancing measures at airports and on-board aircraft, enhanced hygiene and cleaning [3].
In most countries, once the virus has been introduced into the community, imported cases are likely to
contribute little to the ongoing spread of SARS-CoV-2.
Air travellers should be considered as a mostly non-symptomatic subpopulation with a low probability of being
infected with COVID-19, comparable to the general population of the country of origin.
Competent authorities and the relevant stakeholders should ensure that the non-pharmaceutical interventions
(NPI) outlined in the COVID-19 Aviation Health Safety Protocol are implemented and that passenger locator
forms (PLF) are completed and collected in order to enable efficient contact tracing.
Air travellers should be duly informed of all the measures in place.
Entry screening, quarantine and border closures for incoming travellers are unlikely to prevent the introduction
of SARS-CoV-2 into a community, although they might delay it for a short period of time. However, public
health capacity must be in place to mitigate the risk of the introduction of SARS-CoV-2 and prevent further
transmission.
Implementing systematic testing for SARS-CoV-2 of air travellers is not recommended, except in specific
epidemiological scenarios (see below), as it may detract public health resources and laboratory capacity from
essential public health activities, such as timely testing of possible cases in the community and high-risk
settings, contact tracing, and cluster investigations.
Decision-makers in the Member States need to ensure that they have sufficient capacity in place for contact-
tracing and all other similar measures.

ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
6
According to the available evidence to date, the spread of SARS-CoV-2 is mostly facilitated by human interactions
in the absence of NPIs such as physical distancing, hand and respiratory hygiene and the use of face masks, with
the majority of the clusters occurring in crowded indoor settings. As regards travellers, it is important to
differentiate them from high-risk close contacts of a confirmed COVID-19 case. Studies have shown that the
prevalence of COVID-19 in household contacts ranges from 4.649.5% [28], while data from contact tracing
activities in Ireland show an overall positivity rate of 15% [95% Confidence Interval (CI) 11% to 20%] [29]. In
contrast, prevalence in travellers is estimated by modelling studies to be much lower, closer to the estimated
prevalence of COVID-19 in the general population at less than 1% [30,31]. The current average estimated point
prevalence of COVID-19 in general populations in the EU/EEA countries and the UK is thought to be less than
2.5%
3
. As these estimates are based on reported cases and general population point prevalence studies, and as
travellers with symptoms are discouraged from travelling, ECDC estimates that the current prevalence of COVID-19
among travellers in the EU/EEA is approximately 1%, although in areas of intense widespread transmission of
SARS-CoV-2, the prevalence among travellers could be higher.
Based on the data on COVID-19 cases reported by EU/EEA countries and the UK to TESSy, we compared the number
of imported cases as specified by the reporting Member State with that of locally-acquired cases from week 23/2020
to week 45/2020.
Figure 1. Locally acquired and imported cases of COVID-19, as reported by the destination country for
eight EU/EEA countries*, weeks 23–45/2020
*Source: TESSy, ECDC.
Country reports from Czechia, Estonia, Finland, Ireland, Italy, Malta, Norway, and Slovakia. Data were included from countries
that had a) ≥70% completeness of TESSy data, when compared with data retrieved by ECDC epidemic intelligence for the same
period (weeks 23 to 45), and b) maximum 35% of missing data in relation to imported cases.
Figure 1 shows that an increase of imported cases in the EU/EEA and the UK was observed during weeks 3134,
representing a relatively important proportion of imported cases during the summer holidays when the total
number of cases was low. However, as testing policies focused on testing travellers during the beginning of the
pandemic and the summer holidays, this proportion is likely to be biased. The proportion of imported cases
decreased in subsequent weeks and in week 45 (last week with available data), imported cases only accounted for
less than 1% of the total number of cases, with the vast majority of cases being locally acquired, which is
consistent with the current community transmission of COVID-19 in Europe.
3
Based on the highest 14-day notification rate of 1.9% during week 47 and general population PCR point-prevalence estimates
of less than 2%.

ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
7
2.2 Testing and quarantine measures for air travel
Travel restrictions are regulated under the International Health Regulations (IHR) and EU law. In both cases, public
safety and health threats related to infectious disease outbreaks are considered reasonable grounds for Member
States to restrict free movement across borders.
Travel-related measures refer to a variety of measures at Points of Entry (PoE) in response to the COVID-19
outbreak, with the aim of controlling the spread of the disease. Providing information to travellers about the
disease, the epidemiological situation in the destination country and the measures in place is very important and
should be part of the risk communication strategy. In addition, Passenger Locator Forms (PLF) are recommended
as an important tool to facilitate prompt contact tracing in the destination country. The effectiveness of other entry
screening methods, such as temperature screening and health questionnaires, is not supported by evidence [32].
ECDC and EASA strongly recommend the advance provision of information to travellers, a simplified procedure for
obtaining PLFs, preferably in digital format, and the implementation of a combination of NPIs [33] in the
communities, including at airports and on-board airplanes, as set out in the COVID-19 Aviation Health Safety
Protocol.
An overview of travel-related measures for air travel with their advantages and disadvantages is provided in Annex
1. This document focuses on the following travel-related measures: testing of air travellers for SARS-CoV-2 and
quarantine of air travellers.
2.2.1 Testing of air travellers
Testing methods used for the diagnosis of COVID-19 include molecular (RT-PCR or RT-LAMP) and rapid antigen
detection tests (RADTs). RADTs aim to detect active infections (i.e. infectious individuals at the time of testing.)
RT-PCR may also detect non-infectious cases due to the prolonged existence of viral ribonucleic acid (RNA).
No diagnostic test provides 100% sensitivity and specificity; test performance depends on factors such as technical
characteristics of the test, the prevalence of the infection in the target population, the timing of testing, the quality
of the sample, the person’s infection and immune status and the transport of specimens [34]. Proper interpretation
of test results is important for accurate case management. Taking into consideration the measures already
implemented (information to passengers and AHSP guidelines), air travellers are a mostly non-symptomatic
subpopulation, with variable but decreased probability of COVID-19 compared to the general population (estimated
prevalence of COVID-19 in travellers is approximately 1%) [35]. Test performance characteristics
(sensitivity/specificity) and the prevalence of the disease in the target population play a pivotal role in determining
the validity (i.e. ability to detect true positives and true negatives) of the test results. This document is, however,
based on current evidence regarding the existing tests, and further technological developments may require it to
be updated accordingly.
In order to ensure the expected quality of the test and for safety reasons, testing should always be conducted in
accordance with manufacturer’s instructions. Professional sampling is particularly important in the context of testing
Testing and quarantine of travellers are appropriate measures to delay the importation in an area where
SARS-CoV-2 is not yet circulating, or once a country or a region has managed to decrease COVID-19 levels to
almost zero.
Every testing and/or quarantine strategy leaves some residual risk of importation of COVID-19. Member States
should assess what residual risk they are prepared to accept, then manage potential imported cases at
national level through public health infrastructure (e.g. testing of suspected cases, contact tracing and
isolation and provision of healthcare services.)
All available testing methods for COVID-19 have limitations and their performance depends on multiple
factors, including the prevalence of the infection in the target population.
Tests will not detect individuals that are incubating the disease at the time of testing or have viral loads below
the level of detection of the testing method used.
If screening of travellers is being considered, Member States should aim for the use of RT-PCR tests or other
tests with performance close to RT-PCR.
RADTs perform best in cases with high viral load, in early symptomatic cases up to five days from symptom
onset.
Where a country or an area has achieved consistent sustained control of SARS-CoV-2, with a 14-day incidence
close to zero, RADTs are not suitable for screening incoming travellers to prevent virus introduction or re-
introduction. In these situations, only RT-PCR should be used to reduce the risk of false negative results.
According to modelling studies, testing can help shorten the duration of quarantine.

ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
8
with rapid antigen tests as the test lacks a control showing successful sampling. When testing at the PoE, trained
healthcare or laboratory staff, or trained operators are needed to carry out sampling, testing, test analysis and
reporting of test results to clinical staff and public health authorities at local, regional, national and international level.
Self-testing may be an option if included in the manufacturer’s instructions, provided that time and appropriate facilities
are planned. When considering testing of travellers, Member States should give proper consideration to availability and
prioritisation of all prerequisite resources, including appropriate human resources. The use of any diagnostic test for
screening purposes, including RT-PCR and RADT, in a low prevalence population can lead to a number of false negative
and false positive results, which would be higher for the RADT method. False negative cases pose a risk of importation
and transmission during travel, while the false positives would require proper management until the result of the
confirmation test is received. The management of the positive cases is expected to have an impact on the public health
capacity as well as on aircraft and aerodrome operators, if testing is organised at airport premises.
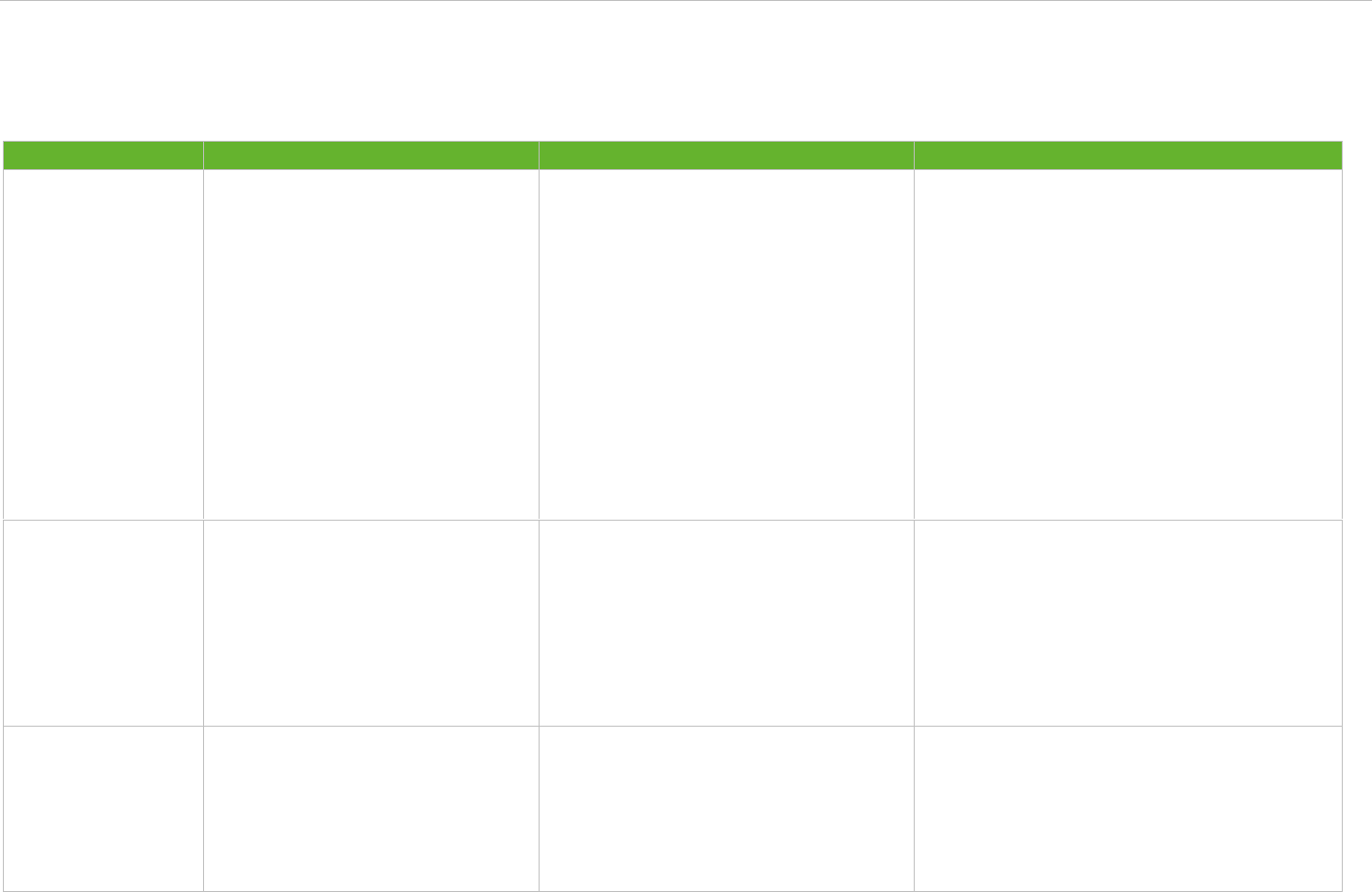
Table 1 shows the true and false positive results expected if testing is implemented in air traveller population. As
illustrated, the use of a low-performance test (with a sensitivity of 80% and specificity of 97%) would lead to more
false positive (FP) and false negative (FN) results when compared to a high-performance test (with sensitivity of 95%
and specificity of 98%). False positive cases are indistinguishable from true positives, unless a more specific test or
repeat testing is performed for confirmation. Both false positive and false negative cases have public health
implications. In the case of false positives, these individuals will have to be isolated and they will trigger contact
tracing activities and further testing (i.e. requiring additional public health resources.) False negative cases, on the
other hand, will give a false sense of security while triggering chains of community transmission. Therefore, the
inherent risk of missing positive cases and the need to mobilise public health resources for false positive cases needs
to be carefully considered when contemplating systematic testing. If systematic testing of air travellers is
implemented then, as illustrated in these examples, it is critical to use clinically validated tests with high performance,
which is as close as possible to RT-PCR performed in laboratories, and to ensure a rapid turnaround of test results.
Table 1. Test results when using high and low performing tests in air traveller population [35,36]
Examples of
COVID-19
prevalence
in the
travellers
Aviation related
target group tested
Test
characteristics
(High†/Low‡
performing test)
Test results*
True
positive
(TP)
False
positive
(FP)
True
negative
(TN)
False
negative
(FN)
0.5%
Average intra-EU flight:
180 travellers
H
1
4
176
0
L
1
5
174
0
Passenger volume per
day at an EU airport:
20 000 travellers
H
95
398
19 502
5
L
80
597
19 303
20
Passenger volume per
day at an EU airport:
5 000 travellers
H
24
100
4 876
1
L
20
149
4 826
5
1.5%
Average intra-EU flight:
180 travellers
H
3
4
174
0
L
2
5
172
1
Passenger volume per
day at an EU airport:
20 000 travellers
H
285
394
19 306
15
L
240
591
19 109
60
Passenger volume per
day at an EU airport:
5 000 travellers
H
71
99
4 827
4
L
60
148
4 777
15
3.0%
Average intra-EU flight:
180 travellers
H
5
3
171
0
L
4
5
169
1
Passenger volume per
day at an EU airport:
20 000 travellers
H
570
388
19 012
30
L
480
582
18 818
120
Passenger volume per
day at an EU airport:
5 000 travellers
H
143
97
4 753
8
L
120
146
4 705
30
*Results are rounded to the nearest whole number as they refer to persons, consequently the sum of the columns approximates
the total number of passengers; †High- performance test: 95% sensitivity, 98% specificity; ‡Low-performance test: 80% sensitivity,
97% specificity, TP: true positive, FP: false positive, TN: true negative, FN: false negative.

ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
9
Molecular tests for screening air travellers
Reverse transcription polymerase chain reaction (RT-PCR) has until now been the mainstay and the gold standard in
terms of SARS-CoV-2 testing.
RT-PCR has the characteristics set out below:
It detects the genetic material of the SARS-CoV-2 virus.
It is a diagnostic test with high sensitivity, usually higher than 95%, and very high specificity 99100%.
A SARS-CoV-2 positive RT-PCR test does not necessarily mean that the tested person is infectious since
recovering cases can remain RT-PCR positive for weeks.
Although RT-PCR will very seldom miss a positive case, some false negative results can occur in cases with
low viral load or improper pre-analytical conditions (e.g. sampling technique or poor swab quality).
False positive results are rare but can occur in very low prevalence settings or in any setting in the event of
contamination issues.
Reverse transcription loop-mediated isothermal amplification (RT-LAMP) technique has emerged as an alternative
molecular detection method for the detection of SARS-CoV-2. RT-LAMP technique has some advantages such as
fast test results and need of fewer resources, while maintaining high sensitivity and specificity [37]. Proper clinical
validation studies are needed to evaluate this new technique and assess the potential role it could play in the travel
setting.
Rapid Antigen Detection Tests (RADTs) for screening air travellers
RADTs have the following characteristics:
Rapid antigen tests perform best in cases with high viral load, in pre-symptomatic and early symptomatic
cases up to five days from symptom onset [38].
The use of rapid antigen tests can be recommended for testing individuals irrespective of symptoms in
settings where the proportion of test positivity is expected to be equal to or higher than 10% [38].
Rapid Antigen Detection Tests (RADTs) can provide a result within 1030 minutes, allowing rapid turnaround
of results and shortening the time before further contact tracing and self-isolation can begin.
Some rapid antigen tests require a laboratory instrument for the analysis, but others do not as the analysis is
performed on a handheld cartridge with visual readout.
RADTs have by nature of their technology a lower sensitivity than RT-PCR test for detecting SARS-CoV-2 and
therefore a lower positive predictive value. In a low prevalence population, such as travellers, screening of
asymptomatic persons by RADTs is not recommended and therefore, if such screening is to be attempted by
Member States, RT-PCR tests should be used instead [38].
Validation studies for RADTs are ongoing, while a number of EU/EEA countries are piloting these tests in various
settings, including at airports and PoE [38,39]. Several key principles should be taken into consideration before
deploying RADTs for public health purposes [40,41].
When using RADTs, appropriate biosafety measures must be in place, and a risk assessment performed when
sampling, handling and processing specimens and tests.
Manufacturer instructions for sample collection, specimen type, safe handling, proper waste management and
intended use need to be followed precisely at all times.
The current recommended use is for individuals with high viral loads. RADTs may miss individuals with low
viral loads, for example during the pre-symptomatic phase and/or towards the end of the active infection.
Test performance data play a significant role in test selection; ideally the test used should have undergone
independent clinical evaluation (e.g. by the FIND foundation) [35].
The sensitivities and specificities of RADTs currently range from 29% to 93.9% for test sensitivity and from
80.2% to 100% for test specificity, depending on the time of sampling [38].
RADTs should be able to rule out most infectious cases. In a low-prevalence population, such as travellers,
and if tested by RADTs, a positive test will need confirmation by RT-PCR.
A negative result from an RADT should not be used to inform decisions on discontinuation of quarantine,
which is based on the duration of the incubation period.
RADTs may be useful for diagnosing suspected cases (e.g. travellers who suddenly develop COVID-19
compatible symptoms.)
RADTs are not suitable for screening incoming travellers to prevent virus (re-)introduction in
regions/countries that have achieved zero or very low levels of transmission. In these situations (i.e. in a low
prevalence population), only RT-PCR should be used to reduce the risk of false negative results.
A number of the EU/EEA countries have implemented requirements for a recent negative COVID-19 RT-PCR test
result in order to allow entry into their territory. According to modelling studies, performing a single RT-PCR test
immediately upon arrival would prevent only 40% to 50% of local transmission from imported cases [30,42,43].
Furthermore, modelling studies have shown that pre-flight testing is less effective in preventing the importation of
the virus than a similar test performed upon arrival. The longer the time between the sample collection from a

ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
10
person without symptoms for a pre-flight test and the scheduled time of departure, the less effective the test will
be. If a pre-departure negative test is requested, the sample should ideally be collected within 48 hours before
departure [34]. Pre-departure testing reflects the situation of the tested individuals on the day the test is
performed and cannot guarantee that they will not become positive in the immediate future. However, pre-
departure testing may reduce the chances of transmission during travel, especially from areas with very high
transmission levels. If a Member State is considering the introduction of pre-departure testing, it should also
provide travellers with the possibility to undertake a test upon arrival [6].
Finally, implementing a testing procedure at airports may increase crowding, thus creating opportunities for SARS-
CoV-2 transmission. Therefore if such testing is attempted by a Member State, it is recommended that the logistics
for testing at PoE be carefully organised to ensure physical distancing and the protection of staff at all times.
2.2.2 Quarantine of air travellers
Many EU/EEA countries and the UK have adopted quarantine as a measure for incoming travellers, assuming that
some of these travellers may be incubating the disease or have the disease but are asymptomatic. Some of the EU
countries are making exceptions for short-term travellers (i.e. expected return within 72 hours). Quarantine for
travellers will probably have an impact on their ability to work and provide for their family and it may affect their
mental health. In addition, and according to the experience until now, these factors vary significantly depending on
socio-economic status and age.
Travellers should be treated as local residents of the destination country and the same recommendations on how
to prevent spread should apply to them, in accordance with local public health guidance.
The requirement for incoming travellers to quarantine, as a separate measure from quarantine of contacts, should
be communicated to travellers by the country of destination well before their travel date, so that they have the
opportunity to prepare. When implementing quarantine on entry, the country should provide adequately equipped
quarantine facilities for travellers that have no possibility of home quarantine. Countries should also explore options
for quarantine monitoring measures, such as daily health checks, or follow-up calls, according to their national
capacities.
Data on compliance with quarantine rules are not readily available for the EU/EEA countries and the UK.
Decreasing the duration of quarantine could, in theory, facilitate compliance. Moreover, there are currently no
empirical data available on the effectiveness of shortened quarantine duration. At this point, only modelling studies
(still in pre-print) provide information on the effectiveness of different durations of quarantine, alone or in
combination with testing, to prevent the importation of COVID-19 cases [30,42,43]. An overview of these
modelling studies is provided in Annex 3.
Quarantine of travellers may be an effective public health measure to delay the importation and/or limit
reintroduction of SARS-CoV-2, if implemented comprehensively and very early in the evolution of the epidemic
situation or when a country has reduced transmission levels to close to zero. Examples of the implementation of
this approach are countries such as Taiwan and New Zealand [44,45]. In the current epidemiological situation,
where SARS-CoV-2 is established in the communities of all EU/EEA countries and the UK, imported cases account
for a very small proportion of all detected cases and are unlikely to contribute significantly to increased
transmission (Figure 1).
2.2.3 Combination of testing and quarantine for air travellers
An approach used by several countries is to combine quarantine with the testing of incoming travellers in order to
reduce quarantine duration.
According to data provided by 30 countries in the EU/EEA and the UK until 16 October 2020, 12 countries (40%)
require 14-day quarantine or a combination with testing at one, five or seven days after arrival for travellers from
certain countries. Five out of 30 countries require 10 days quarantine and/or testing after arrival; one Member
State recommends a seven-day quarantine and testing before release and one requires two tests 48 hours apart.
Lack of harmonisation and frequent, sometimes sudden, changes in national policies are causing confusion and
having a deterrent effect on travel.
When assessing an appropriate quarantine duration, it is important to differentiate between contacts of a
confirmed case and travellers [29,46]. Travellers, as mentioned above, represent a specific population, who are not
by definition contacts of a COVID-19 confirmed case, unless they had been in contact. Risk communication is
ongoing by public health authorities and aviation stakeholders to emphasise the importance of not travelling with
COVID-19-compatible symptoms or, if identified as high-risk contact of a confirmed case. This remains one of the
most effective ways to reduce the risk of transmission during travel and upon arrival. Available evidence does not
support quarantine and testing of travellers as an effective public health measure which will substantially reduce
overall transmission in the general population (other than in the exceptional situation described above, when a
country has reduced transmission levels to close to zero).

ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
11
Modelling studies (still in pre-print) [30,42,43] have explored different aspects of the effectiveness of various
combination strategies in detecting imported cases of COVID-19, as outlined in Annex 3. Based on these studies, a
14-day quarantine period appears to be most effective in reducing the risk of transmission from travellers,
although this creates logistical and financial challenges. A 10-day quarantine (without testing at day 10) seems to
be the next most effective alternative, particularly if used in combination with other non-pharmaceutical
interventions or where countries do not have enough testing capacity.
Alternatives involving shortened quarantine or combinations of quarantine and testing have been also explored,
and it is expected that these will have less negative social impact. If a Member State implements quarantine of
travellers, testing could help shorten the quarantine period. A single test upon arrival is considered to be about 40
to 50% effective in preventing the importation of the virus. Given the likely low prevalence of infection among
travellers, and assuming that contact information is collected for travellers to enable follow-up if required, the
combination of quarantine and a single test at around day 7 after arrival appears to offer a reasonable balance of
risks and benefits as an alternative to longer quarantine without testing. However, this requires sufficient testing
capacity. Testing twice (upon arrival and after a few days to release from quarantine) does not seem to
significantly increase effectiveness - compared to testing only once to release from quarantine - and it is logistically
challenging and more resource intensive.
Further details regarding the expected residual risk for various combinations are set out in Annex 3.
3. Operational recommendations
Importation of COVID-19 can occur from any point of origin where there is ongoing transmission, including another
area in the same country. The majority of EU/EEA countries and the UK are currently experiencing widespread
transmission of COVID-19 [47]. Therefore, the relative significance of the virus being introduced by cross-border
travellers is minimal compared to ongoing community transmission and transmission related to national/non-cross-
border travel.
Calculations from modelling studies show that all possible combinations of quarantine duration, including for 14
days, with and without testing, still involve a residual risk of cases being imported. This residual risk - which also
depends on the volume of travellers and the prevalence of the disease in their place of origin - should be
addressed by ensuring that public health measures are in place in the community to reduce opportunities for
transmission at all times. These include NPIs, as recommended for air travel in the COVID-19 AHSP, and solid
public health infrastructure, such as sufficient testing capacity for suspected cases and rapid turnaround of results,
contact tracing and isolation/quarantine capacities. Given the estimated low prevalence of COVID-19 among
travellers and the limited public health impact of detecting a few cases among travellers, performing systematic
testing of travellers to reduce the risk of importation may not be the most effective use of public health resources.
When assessed according to the criteria set out in the Council Recommendation (EU) 2020/1475, most of the areas
in the EU/EEA countries and the UK are currently classified as red
4
. At this stage, efforts should be focused on
effective data collection via passenger locator forms (PLF) - where possible digitalised - to support contact tracing
capacities in the community, increased testing for suspected cases and the coordination of communication between
aviation stakeholders and public health authorities.
4
The adopted thresholds indicate that areas in EU/EEA countries and the UK are marked in the following colours:
Green, if the 14-day notification rate is lower than 25 cases per 100 000 and the test positivity rate below 4%.
Orange, if the 14-day notification rate is lower than 50 cases per 100 000 but the test positivity rate is 4% or higher or, if
the 14-day notification rate is between 25 and 150 cases per 100 000 and the test positivity rate is below 4%.
Red, if the 14-day notification rate is 50 cases per 100 000 or higher and the test positivity rate is 4% or higher or if the
14-day notification rate is higher than 150 cases per 100 000.
Grey, if there is insufficient information or if the testing rate is lower than 300 cases per 100 000.

ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
12
5
This refers to the situation at the time of publication. Depending on the evolution of the pandemic and future evidence,
including risk assessment criteria, this document will be updated accordingly.
6
At the time of writing, community transmission is occurring in all EU/EEA MS and the UK; once countries have reduced
transmission levels to close to zero this may need to be reconsidered.
Based on existing evidence and information available, as presented in this document,
ECDC and EASA offer the following recommendations
1. Available evidence does not support quarantine and testing of travellers as an effective public health measure to substantially
reduce overall transmission in the general population, except when a country has reduced transmission levels to almost zero.
Particularly in the current epidemiological situation
5
, systematic testing for SARS-CoV-2 and/or quarantine of air travellers is
not recommended [25]. A pre-flight test could reduce the possibility of transmission during travel, especially when departure
is from a country or an area with very high incidence rates. Once the epidemiological situation has improved, if countries are
considering the adoption of screening or quarantine of incoming travellers, the following possible approaches – schematically
summarised in Annex 2 – should be taken into account.
When travel is taking place from a lower-risk to a higher-risk area or between areas of similar risk, there is no
public health benefit in testing for SARS-CoV-2 and/or quarantine of travellers before departure or upon arrival in
the destination country.
Exceptionally, for travel between two high-risk areas, when travel begins from a very high-incidence area, a
combination of testing and shortened quarantine could be considered, although this requires sufficient testing capacity.
When travel is from an area of high or unknown risk to a lower-risk area, based on modelling studies, a combination of
testing and shortened quarantine could be considered, if sufficient testing capacity is available.
2. Where a country or an area has achieved consistent sustained control of the virus, having a 14-day incidence close to zero, all
incoming individuals from regions with community transmission should be tested before entering the COVID-19-free areas.
Given the 14-day incubation period and the possibility of asymptomatic disease, these travellers should undergo quarantine
(voluntary or mandatory) and be tested rapidly if they develop COVID-19 compatible symptoms. In the absence of symptoms,
they should be tested again at the end of the quarantine period [48].
When implementing the above recommendations, Member States should also give proper consideration to the principles below:
Persons with COVID-19 compatible symptoms - or contacts of a confirmed or probable case [1] – should be
discouraged from travelling by means of appropriate measures, including health safety promotion and risk
communication.
In view of the current epidemiological situation in the EU/EEA countries and the UK
6
, considering the potentially
reduced opportunity for infection for people travelling for short periods (i.e. expected return within 72 hours) and where
contacts with local population are limited, countries may consider exemptions from quarantine and/or SARS-CoV-2
testing for such travellers, unless they exhibit COVID-19-compatible symptoms.
Transiting passengers should not be tested in the country of transfer, with the exception of cases developing COVID-
19-compatible symptoms during travel. If countries require information on the test results for transiting passengers,
they should accept that testing can be done either before departure from the country of origin or upon arrival at the
final destination, in which case information on positive cases can be exchanged via the PLF system.
Tests with high-performance characteristics should be preferred. Optimally, Member States should aim for the use of RT-
PCR tests or other tests with performance close to RT-PCR, as prevalence of COVID-19 is expected to be low among air
travellers, and using lower performance tests would result in a significant number of false (positive and negative) results.
Tests used should be validated and performed by appropriately trained personnel to maintain quality and testing
standards.
Children under two years of age should be exempt from testing. For children above the age of two, Member States may
consider alternative validated sample collection methods.
Testing at Points of Entry should not be prioritised over community and healthcare needs.
Test results should preferably be delivered in a reliable electronic format, which enables easy reading of the result and
prevents fraud attempts.
Testing requirements for travellers implemented by Member States should be notified to the European Commission and
the other Member States in order to facilitate mutual recognition in accordance with the Council Recommendation (EU)
2020/1475.
If testing at airport premises is implemented, the competent national or local authorities and the relevant stakeholders should
also make arrangements, as described below.
Organise testing facilities at PoE in terms of logistics to ensure physical distancing and the protection of staff and
travellers at all times.
Develop appropriate policies for the management of positive cases describing the processes for a confirmation test,
quarantine and transport to the quarantine location.
Develop, in coordination with the aircraft and aerodrome operators, policies and procedures relating to the denial of
boarding for travellers who test positive in accordance with the relevant EU requirements. Furthermore, aircraft
operators should enable refund or free rebooking for those travellers who have tested positive (and their close
contacts/travel companions.)

ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
13
In line with the guidance set out in the Council Recommendation (EU) 2020/1475 [6], any travel-related measures
put in place should be proportionate and non-discriminatory, focusing on what is necessary for the protection of
public health. The Member States should always admit their own nationals and Union citizens and their family
members resident in their territory and facilitate swift transit through their territories. Finally, the Member States
should ensure that their travel-related measures are well communicated and coordinated to facilitate compliance
by the travellers.
Contributing ECDC experts (in alphabetical order)
Agoritsa Baka, Eeva Broberg, Orlando Cenciarelli, Bruno Ciancio, Margot Einöder-Moreno, Francesco Innocenti,
Csaba Ködmön, Annette Kraus, Katrin Leitmeyer, Angeliki Melidou, Dominique Monnet, Lina Nerlander, Diamantis
Plachouras, Emmanuel Robesyn, Gianfranco Spiteri, Carl Suetens.
Contributing EASA experts (in alphabetical order)
Ana Dedijer, Cristian Ionut Panait.
ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
14
References
1. European Centre for Disease Prevention and Control (ECDC). Contact tracing: public health management of
persons, including healthcare workers, who have had contact with COVID-19 cases in the European Union –
third update [updated 18 November 2020]. Available at: https://www.ecdc.europa.eu/en/covid-19-contact-
tracing-public-health-management
2. EUR-Lex.europa.eu. Consolidated version of the Treaty on the Functioning of the European Union [cited 22
November 2020]. Available at: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex%3A12012E%2FTXT
3. European Union Aviation Safety Agency (EASA) and European Centre for Disease Prevention and Control
(ECDC). COVID-19 Aviation Health Safety Protocol [updated 30 June 2020]. Available at:
https://www.easa.europa.eu/document-library/general-publications/covid-19-aviation-health-safety-protocol
4. European Union (EU). Re-open EU. [cited 20 October 2020]. Available from: https://reopen.europa.eu/en
5. European Commission (EC) - Directorate-General for Health and Food Safety. EU health preparedness:
Recommendations for a common EU testing approach for COVID-19 [cited 22 November 2020]. Available at:
https://ec.europa.eu/health/sites/health/files/preparedness_response/docs/common_testingapproach_covid-
19_en.pdf
6. Council of the European Union. Draft Council Recommendation on a coordinated approach to the restriction of
free movement in response to the COVID-19 pandemic [updated 12 October 2020]. Available at:
https://data.consilium.europa.eu/doc/document/ST-11689-2020-REV-1/en/pdf
7. European Commission (EC). Communication from the Commission to the European Parliament, the European
Council and the Council on additional COVID-19 response measures [updated 28 October 2020]. Available at:
https://ec.europa.eu/info/sites/info/files/communication-additional-covid-19-response-measures.pdf
8. European Commission (EC). Commission Recommendation of 28.10.2020 on COVID-19 testing strategies,
including the use of rapid antigen tests [cited 22 November 2020]. Available at:
https://ec.europa.eu/health/sites/health/files/preparedness_response/docs/covid19_testingstrategies_recom
mendation_en.pdf
9. Polgreen PM, Polgreen EL. Emerging and Re-emerging Pathogens and Diseases, and Health Consequences of
a Changing Climate. Infectious Diseases. 2017;1:40-8.e2. Available at: https://doi.org/10.1016/B978-0-7020-
6285-8.00004-6
10. St John RK, King A, de Jong D, Bodie-Collins M, Squires SG, Tam TW. Border screening for SARS. Emerg
Infect Dis. 2005 Jan;11(1):6-10. Available at: https://wwwnc.cdc.gov/eid/article/11/1/04-0835_article
11. Hung KKC, Mark CKM, Yeung MPS, Chan EYY, Graham CA. The role of the hotel industry in the response to
emerging epidemics: a case study of SARS in 2003 and H1N1 swine flu in 2009 in Hong Kong. Globalization and
Health. 2018;14(1):117. Available at:
https://globalizationandhealth.biomedcentral.com/articles/10.1186/s12992-018-0438-6
12. Correa-Martínez CL, Kampmeier S, Kümpers P, Schwierzeck V, Hennies M, Hafezi W, et al. A pandemic in
times of global tourism: superspreading and exportation of COVID-19 cases from a ski area in Austria. Journal
of Clinical Microbiology. 2020;58(6):e00588-20. Available at: https://jcm.asm.org/content/58/6/e00588-20
13. Linka K, Peirlinck M, Sahli Costabal F, Kuhl E. Outbreak dynamics of COVID-19 in Europe and the effect of
travel restrictions. Computer Methods in Biomechanics and Biomedical Engineering. 2020;23(11):710-7.
Available at: https://www.tandfonline.com/doi/full/10.1080/10255842.2020.1759560
14. Quilty BJ, Diamond C, Liu Y, Gibbs H, Russell TW, Jarvis CI, et al. The effect of travel restrictions on the
geographical spread of COVID-19 between large cities in China: a modelling study. BMC Med. 2020;18(259).
Available at: https://doi.org/10.1186/s12916-020-01712-9
15. Grüll P. How an Austrian ski paradise became a COVID-19 hotspot [cited 12 May 2020]. Available at:
https://www.euractiv.com/section/coronavirus/news/ischgl-oesterreichisches-skiparadies-als-corona-hotspot/
16. Yang Y, Zhang H, Chen X. Coronavirus pandemic and tourism: Dynamic stochastic general equilibrium
modeling of infectious disease outbreak. Annals of Tourism Research. 2020;83:102913. Available at:
https://doi.org/doi:10.1016/j.annals.2020.102913
17. Apolone G, Montomoli E, Manenti A, Boeri M, Sabia F, Hyseni I, et al. Unexpected detection of SARS-CoV-2
antibodies in the prepandemic period in Italy. Tumori [Preprint]. 11 November 2020. Available at:
https://journals.sagepub.com/doi/10.1177/0300891620974755
18. Quilty BJ, Clifford S, Flasche S, Eggo RM. Effectiveness of airport screening at detecting travellers infected
with novel coronavirus (2019-nCoV). Euro Surveill. 2020 Feb;25(5). Available at:
https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2020.25.5.2000080
19. Clifford S, Pearson CAB, Klepac P, Van Zandvoort K, Quilty BJ, group CC-w, et al. Effectiveness of
interventions targeting air travellers for delaying local outbreaks of SARS-CoV-2. Journal of Travel Medicine.
2020;27(5). Available at: https://academic.oup.com/jtm/article/27/5/taaa068/5834629
20. Russell TW, Wu J, Clifford S, Edmunds J, Kucharski AJ, Jit M. The effect of international travel restrictions on
internal spread of COVID-19. medRxiv [Preprint] 14 July 2020. Available at:
https://doi.org/10.1101/2020.07.12.20152298

ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
15
21. Riccardo F, Ajelli M, Andrianou X, Bella A, Del Manso M, Fabiani M, et al. Epidemiological characteristics of
COVID-19 cases in Italy and estimates of the reproductive numbers one month into the epidemic. medRxiv
[Preprint]. 11 April 2020. Available at: https://doi.org/10.1101/2020.04.08.20056861
22. Wei Y, Wei L, Liu Y, Huang L, Shen S, Zhang R, et al. A systematic review and meta-analysis reveals long and
dispersive incubation period of COVID-19. medRxiv [Preprint] 20 June 2020. Available at:
https://doi.org/10.1101/2020.06.20.20134387
23. Gámbaro F, Behillil S, Baidaliuk A, Donati F, Albert M, Alexandru A, et al. Introductions and early spread of
SARS-CoV-2 in France, 24 January to 23 March 2020. Euro Surveill. 2020 Jul;25(26). Available at:
https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2020.25.26.2001200
24. Samaan G, Patel M, Spencer J, Roberts L. Border screening for SARS in Australia: what has been learnt? Med
J Aust. 2004 Mar 1;180(5):220-3. Available at: https://onlinelibrary.wiley.com/doi/abs/10.5694/j.1326-
5377.2004.tb05889.x
25. European Centre for Disease Prevention and Control (ECDC). Entry and exit screening measures [updated 12
October 2014]. Available at:
https://www.ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/Ebola-outbreak-
technicalreport-exit-entry-screening-13Oct2014.pdf
26. Murphy N, Boland M, Bambury N, Fitzgerald M, Comerford L, Dever N, et al. A large national outbreak of
COVID-19 linked to air travel, Ireland, summer 2020. Euro Surveill. 2020;25(42). Available at:
https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2020.25.42.2001624
27. Freedman DO, Wilder-Smith A. In-flight transmission of SARS-CoV-2: a review of the attack rates and
available data on the efficacy of face masks. Journal of Travel Medicine [Preprint]. 25 September 2020.
Available at: https://doi.org/10.1093/jtm/taaa178
28. Shah K, Saxena D, Mavalankar D. Secondary attack rate of COVID-19 in household contacts: a systematic
review. QJM [Preprint] 29 July 2020. Available at: https://doi.org/10.1093/qjmed/hcaa232
29. Health Information and Quality Authority (HIQA). Potential impact of different testing scenarios to reduce the
duration of restriction of movement for close contacts of a COVID-19 case [updated 4 November 2020].
Available at: https://www.hiqa.ie/sites/default/files/2020-11/Potential-impact-of-different-testing-scenarios-
to-reduce-the-duration.pdf
30. Clifford S, Quilty BJ, Russell TW, Liu Y, Chan Y-WD, Pearson CA, et al. Strategies to reduce the risk of SARS-
CoV-2 re-introduction from international travellers. medRxiv [Preprint] 25 July 2020. Available at:
https://doi.org/10.1101/2020.07.24.20161281
31. Russell TW, Hellewell J, Abbott S, Golding N, Gibbs H, Jarvis CI, et al. Using a delay-adjusted case fatality
ratio to estimate under-reporting [cited 23 November 2020]. Available at:
https://cmmid.github.io/topics/covid19/global_cfr_estimates.html
32. European Centre for Disease Prevention and Control (ECDC). Considerations for travel-related measures to
reduce spread of COVID-19 in the EU/EEA [updated 26 May 2020]. Available at:
https://www.ecdc.europa.eu/en/publications-data/considerations-travel-related-measures-reduce-spread-
covid-19-eueea
33. European Centre for Disease Prevention and Control (ECDC). Guidelines for the implementation of non-
pharmaceutical interventions against COVID-19 [updated 24 September 2020]. Available at:
https://www.ecdc.europa.eu/en/publications-data/covid-19-guidelines-non-pharmaceutical-interventions
34. Sethuraman N, Jeremiah SS, Ryo A. Interpreting Diagnostic Tests for SARS-CoV-2. JAMA. 2020 Jun
9;323(22):2249-51. Available at: https://jamanetwork.com/journals/jama/fullarticle/2765837
35. FIND. Rapid Diagnostic Tests for COVID-19 [updated 18 May 2020]. Available at: https://www.finddx.org/wp-
content/uploads/2020/05/FIND_COVID-19_RDTs_18.05.2020.pdf
36. Watson J, Whiting PF, Brush JE. Interpreting a covid-19 test result. BMJ. 2020;369:m1808. Available from:
https://www.bmj.com/content/bmj/369/bmj.m1808.full.pdf
37. Dao Thi VL, Herbst K, Boerner K, Meurer M, Kremer LP, Kirrmaier D, et al. A colorimetric RT-LAMP assay and
LAMP-sequencing for detecting SARS-CoV-2 RNA in clinical samples. Sci Transl Med. 2020;12(556). Available
at: https://stm.sciencemag.org/content/12/556/eabc7075.short
38. European Centre for Disease Prevention and Control (ECDC). Options for the use of rapid antigen tests for
COVID-19 in the EU/EEA and the UK [updated 19 November 2020]. Available at:
https://www.ecdc.europa.eu/en/publications-data/options-use-rapid-antigen-tests-covid-19-eueea-and-uk
39. European Commission (EC). Commission Recommendation of 18.11.2020 on the use of rapid antigen tests for
the diagnosis of SARS-CoV-2 infection [cited 22 November 2020]. Available at:
https://ec.europa.eu/health/sites/health/files/preparedness_response/docs/sarscov2_rapidantigentests_recom
mendation_en.pdf
40. World Health Organization (WHO). Antigen-detection in the diagnosis of SARS-CoV-2 infection using rapid
immunoassays [updated 11 September 2020]. Available at: https://www.who.int/publications/i/item/antigen-
detection-in-the-diagnosis-of-sars-cov-2infection-using-rapid-immunoassays
41. Van Walle I, Leitmeyer K, Broberg EK. Meta-analysis of the clinical performance of commercial SARS-CoV-2
nucleic acid, antigen and antibody tests up to 22 August 2020. medRxiv [Preprint] 18 September 2020.
Available at: https://www.medrxiv.org/content/10.1101/2020.09.16.20195917v1

ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
16
42. Ashcroft P, Lehtinen S, Bonhoeffer S. Quantifying the impact of quarantine duration on COVID-19
transmission. medRxiv [Preprint] 5 October 2020. Available at: https://doi.org/10.1101/2020.09.24.20201061
43. Taylor R, McCarthy CA, Patel V, Moir R, Kelly L, Snary E. The risk of introducing SARS-CoV-2 to the UK via
international travel in August 2020. medRxiv [Preprint] 9 September 2020. Available at:
https://doi.org/10.1101/2020.09.09.20190454
44. Douglas J, Mendes FK, Bouckaert R, Xie D, Jimenez-Silva CL, Swanepoel C, et al. Phylodynamics reveals the
role of human travel and contact tracing in controlling COVID-19 in four island nations. medRxiv [Preprint].
6 August 2020. Available at: https://doi.org/10.1101/2020.08.04.20168518
45. Jefferies S, French N, Gilkison C, Graham G, Hope V, Marshall J, et al. COVID-19 in New Zealand and the
impact of the national response: a descriptive epidemiological study. Lancet Public Health [Preprint].
14 October 2020; Available at: https://www.sciencedirect.com/science/article/pii/S2468266720302255
46. Quilty BJ, Clifford S, Flasche S, Kucharski AJ, Edmunds WJ, Group CC-W. Quarantine and testing strategies in
contact tracing for SARS-CoV-2. medRxiv [Preprint]. 6 October 2020. Available at:
https://doi.org/10.1101/2020.08.21.20177808
47. European Centre for Disease Prevention and Control (ECDC). Weekly COVID-19 country overview [cited 21
October 2020]. Available at: https://www.ecdc.europa.eu/en/covid-19/country-overviews
48. European Centre for Disease Prevention and Control (ECDC). COVID-19 testing strategies and objectives
[updated 18 September 2020]. Available at: https://www.ecdc.europa.eu/en/publications-data/covid-19-
testing-strategies-and-objectives
ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers.– Addendum to the Aviation Health Safety Protocol
17
Annex 1. Overview of travel-related measures (air travel) with
advantages and disadvantages
Measure
Aim and description
Advantages and evidence
Disadvantages and evidence
RT-PCR testing
before departure or
after arrival at
destination
Aim: To detect confirmed cases
among cross-border travellers.
Passenger is required to undergo an
RT-PCR test within a prescribed time
pre-departure and present a negative
result upon arrival
OR
Passenger is required to undergo an
RT-PCR test upon arrival at Point of
Entry (PoE) or within a prescribed time
after arrival at destination.
Very accurate diagnostic test
(sensitivity: 99–100%; specificity: 99-
100%)
Results usually available within 1224
hours. Shorter turnaround times are
possible, but at increased cost.
Pooled testing can decrease laboratory
burden.
Provides a snapshot on the day of testing;
cannot exclude that the traveller becomes
positive on one of day(s) following the test, or is
exposed to the virus after the test was
performed.
Cannot differentiate infectious from non-
infectious COVID-19 cases.
Use of RT-PCR as a screening test: estimated
effectiveness 39.6% (95% CI 35.2-43.7), or
detection of roughly two out of five infectious
passengers [43].
Relatively high cost, which usually must be paid
by the passenger.
In some EU/EEA countries, travelling may not be
a valid reason for obtaining a RT-PCR test.
The use of fake negative-result certificates has
been reported
Rapid Antigen
Detection Test
(RADT) before
departure or after
arrival at destination
Aim: same as above with a shorter
turnaround time for results.
Passenger is required to undergo an
antigen test, usually upon arrival at
PoE (currently under study as an
option).
Rapid test: results available in 1030
minutes.
RADTs require less or no laboratory
equipment.
The RADTs should be performed by
trained operators.
The test can be performed on-site (at
airport or other holding facility)
Lower cost than RT-PCR.
RADTs are not recommended for screening
asymptomatic persons.
Currently available antigen tests generally have
lower sensitivity (6080%) but similar specificity
(98100 %) to RT-PCR.
Depending on the prevalence of the disease in
the target population, RADTs may give rise to
many false positives and false negatives.
Significant problems for passengers who will
need to undergo RT-PCR for verification.
Quarantine of
incoming travellers
Aim: To prevent transmission of the
virus from undetected cases among
cross-border travellers.
All travellers required to quarantine for
14 days.
If implemented comprehensively at all
PoEs and for all persons entering a
country, it can delay introduction.
Effective if the destination area/country
has achieved very low or zero
transmission.
A supervisory/follow up mechanism is needed.
Logistics and financial implications for countries
and travellers.
Significant barrier for cross-border travellers
The effectiveness of quarantine is estimated as:
- 7 days: 51.3% (95% CI: 47.2-55.7)
- 10 days: 68.8% (95% CI: 65.1-72.9)
- 14 days: 78.0% (95% CI: 74.4-81.6) [43].

ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
18
Measure
Aim and description
Advantages and evidence
Disadvantages and evidence
Combination of
testing and
quarantine
Aim: to prevent introduction of, and
transmission of the virus from, cases
among cross-border travellers.
Passenger may be required to undergo
testing on arrival and/or self-
quarantine for 1, 5, 7 or 10 days and
undergo a second RT-PCR test to be
released.
Shortened quarantine period for
travellers can potentially increase
compliance and facilitate travelling.
Decreases cost.
Residual risk of importation with all
combinations modelled in the literature:
- Testing at airport, quarantine for four days and
test on day 4 after arrival is estimated to be
68.9% effective [43].
- Quarantine for seven days and testing on day
7 is estimated to be 74% effective [43].
- Testing at the airport, quarantine for seven
days and test on day 7 after arrival is estimated
to be 76% effective [43].
- Quarantine of seven days with a test on day 7
and release from quarantine on day 8 after arrival
is estimated to detect 94% of infected travellers
[30].
Entry ban / border
closure
Aim: To prevent entry of cases among
cross-border travellers.
All non-citizen or non-resident
travellers are prevented from entering,
at any PoE in the country.
If implemented comprehensively at all
PoEs and for all persons entering a
country, and if also including blanket
quarantine for all nationals/residents
entering/returning to a country.
Can have a true delay effect; proven in
small island states with a limited number
or well-controlled PoEs [44,45].
Comprehensive implementation is challenging in
a globalised economy as it has implications for
the economic sustainability of the countries.
May have devastating financial effects on
various sectors and the country as a whole.
Logistical barriers to trade and transport of
merchandise including foodstuffs, medicines,
PPE and equipment for the management of the
public health crisis.
Questions of legality when applied to travel
within the EU.

ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
19
Annex 2. Guidelines for travel-related measures air travel
7
7
Based on the classification of the countries of departure and arrival, according to the criteria in Council Recommendation 2020/1475
8
Pre-departure testing for travellers from very high incidence regions/countries could be considered mostly to further reduce the possibility of having a positive case on board
9
Where a country or an area has achieved consistent sustained control of the virus having a 14-day rolling incidence close to zero, all incoming travellers should be tested and follow 14-day quarantine.
10
Based on modelling studies, the combination of quarantine and a single test once at around day 7 after arrival appears to offer a reasonable alternative, although it requires sufficient testing capacity.
*
see footnote 5 above (p.12).
Country or area of departure
Country or area of arrival
Travel-related measures by the country or area of arrival
High risk or unknown risk
8
Low risk
9
None
OR
Combinations
10
of testing and shortened quarantine periods could
be considered
Medium risk
None
OR
Combinations* of testing and shortened quarantine periods could
be considered
High risk or unknown risk
None
OR
where travel is initiated from very high incidence areas,
combinations* of testing and shortened quarantine periods could
be considered.
Medium risk
Low risk
None
Medium risk
None
High risk or unknown risk
None
Low risk
Low risk
None
Medium risk
None
High risk or unknown risk
None

ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
20
Annex 3. Overview of quarantine, testing combinations and
effectiveness in preventing local transmission
Strategies of
quarantine and
testing for travellers
Estimates of residual risk of importation of COVID-19
Advantages
Disadvantages
Combinations of
quarantine and testing
for travellers
Estimated effectiveness
of symptom and risk
screening
Costic et al.
Estimates of COVID-19
infectious travellers per
10.000 travellers entering
the country
Clifford et al. (in
preprint)
Using UK data from July
2020
Effectiveness (%) in
preventing imported COVID-
19 cases
Taylor R et al. (in
preprint)
Using UK data from August
2020
Quantification of local transmission
associated with travel prevented by
quarantine (%)
Ashcroft et al. (in preprint)
NO TESTING
Risk communication to
travellers and admin
measures by aviation
≈30% of
symptomatic
travellers are likely to
fly
1-52 infectious travellers
enter the community
- COVID-19 is estimated to have
asymptomatic course in 1830%
of individuals
- Pre-symptomatic transmission is
well established at two days
before symptom onset.
QUARANTINE ALONE
14-day quarantine,
release without any
testing
0-1% residual risk
(0-2 infectious travellers
enter the community)
21% residual risk
(assuming 80% compliance)
0-1% residual risk
- Difficulty in monitoring
quarantine compliance for
countries.
- Compliance may be lower than
80%.
10-day quarantine,
release without any
testing
31% residual risk
(assuming 80% compliance)
1% residual risk
(assumes also 50% reduction of
transmission due to implemented
NPI measures).
Option for countries that
cannot devote testing capacity
to travellers, if good
compliance can be monitored.
7-day
quarantine, release
without any testing
Up to 20% residual risk
0-13 infectious travellers
enter the community
49% residual risk
(assuming 80% compliance)
It is plausible (although not
supported by evidence) that a
reduction in quarantine
increases compliance.
5-day
quarantine, release
without any testing
Up to 34% residual risk
0-22 infectious travellers
enter the community
3-day quarantine,
release without any
testing
Up to 50% residual risk
1-33 infectious travellers
enter the community

ECDC EASA Guidelines for COVID-19 testing and quarantine of air travellers – Addendum to the Aviation Health Safety Protocol
21
TESTING UPON ARRIVAL
Single RT-PCR test
upon arrival +
quarantine until
receiving the test result
(12 days)
Up to 52% residual risk
1-21 infectious travellers
enter the community
60% residual risk
46% residual risk (assumes also
50% reduction of transmission due
to implemented NPI measures)
†
Significant residual risk, but
countries may accept that some
reduction is better than nothing..
QUARANTINE AND SINGLE TEST
Quarantine + RT-PCR
test on day 7+ release
on day 8 or 9
Up to 16% residual risk
0-6 infectious travellers
enter the community
26% residual risk
Options for countries that wish
to test travellers and can
effectively monitor 7-day
quarantine.
- Challenge for countries to
monitor quarantine compliance.
Quarantine + RT-PCR
test on day 5+ release
on day 6 or 7
Up to 20% residual risk
0-8 infectious travellers
enter the community
Up to 1.5% residual risk
(assumes also 50% reduction of
transmission due to implemented
NPI measures)
Quarantine + RT-PCR
test on day 4 + release
on day 6
36% residual risk
Quarantine + RT-PCR
test on day 3 + release
on day 4
Up to 42% residual risk
0-15 infectious travellers
enter the community
QUARANTINE AND DOUBLE TEST
RT-PCR Test upon
arrival + quarantine +
RT-PCR test on day 7 +
release on day 8
24% residual risk
Options for countries, with
relatively little additional
estimated efficiency, if
compared to single test to
release.
Double testing presents logistics
and resource challenges.
RT-PCR Test upon
arrival + quarantine +
RT-PCR test on day 6 +
release on day 7
<16% residual risk
0-5 infectious travellers
enter the community
RT-PCR Test upon
arrival + quarantine +
RT-PCR test on day 4 +
release on day 5 or 6
Up to 20% residual risk
0-9 infectious travellers
enter the community
31% residual risk
† NPI – non pharmaceutical interventions
- Models use different assumptions and data sets, which may not be generalisable. Please note uncertainty/confidence intervals. Please check the individual publications for the model assumptions.
- Prevalence of COVID-19 in the country of origin plays a significant role.
- Individual burden of quarantine can be psychological and financial. Quarantine has shown to be associated with symptoms of anxiety and post-traumatic stress, longer durations of quarantine were associated with poorer mental
health. (Brooks, The Lancet). Quarantine impact can also be financial and can have lasting impact including on mental health (Brooks, The Lancet). People who work in less secure jobs are particularly vulnerable. Some countries
provide financial aid to people in quarantine.
- Rapid tests (RDTs) are currently not recommended by ECDC for use when releasing asymptomatic people from quarantine.
- Testing used to end quarantine earlier should not compromise access/speed of testing relevant for control, such as testing of symptomatic people or testing of contacts when tracing.
