
Mississippi Medicare Quick Reference Guide
March 2024
wellcare.com/Mississippi/Providers/Medicare
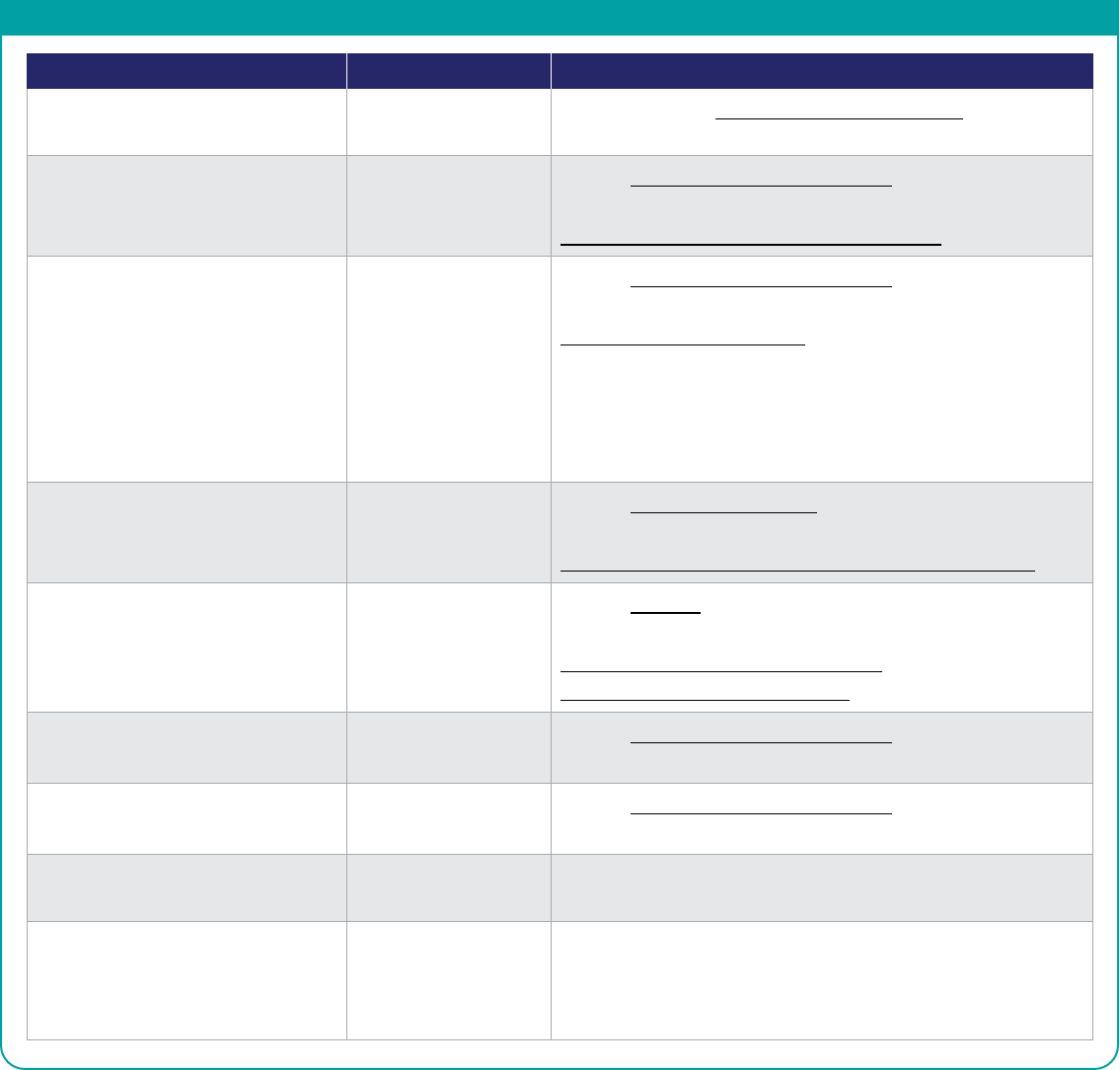
CONVENIENT SELFSERVICE
Wellcare understands that having access to the right tools can help you and your staff streamline day-to-day administrative tasks.
The Provider Portal is the fastest way to get the help with those routine tasks.
Portal Chat (IVR) Interactive Voice Response
Authorization Requirements/Status Fastest Result Available Available
Authorizations Request Fastest Result Available N/A
Benefit/Co-payment Information Fastest Result Available Available
Claims and Appeals Status Fastest Result Available Available
Eligibility Verification Fastest Result Available Available
Submit Appeals/Claims/
Claims Disputes/Corrections
Fastest Result Available N/A
Provider Portal Registration
click here
The portal is not accessible to
non-participating providers. Please
visit our website for information on
Joining our Network.
Provider Portal Training
click here
Provider Services Phone (IVR):
1-855-538-0454 (TTY: 711)
OTHER PHONE NUMBERS
CARE AND DISEASE MANAGEMENT REFERRALS
Phone: 1-866-635-7045 (TTY: 711) | Fax: 1-866-287-3286
Hours: M–F, 8 a.m.–7 p.m. Eastern Standard Time
RISK MANAGEMENT FRAUD, WASTE
& ABUSE HOTLINE
1-866-685-8664
COMMUNITY CONNECTIONS HELP LINE
1-866-775-2192
BEHAVIORAL HEALTH CRISIS LINE
18004116485
24 hours a day for a Behavioral Health Crisis.
For non-crisis related concerns,
members should call Member Services.
NURSE ADVICE LINE
18005819952 (24 hours)
HEALTH PLAN PARTNERS
Contracted Networks
HEARING
HCS
Phone: 1-866-344-7756
VISION
Premier
Phone: 1-833-611-7778
DENTAL
DentaQuest
Phone: 1-833-206-6293
TRANSPORTATION
Medical Transportation Management (MTM)
Phone: 1-888-889-0551
NOTE: Please refer to the member ID card to determine appropriate authorization and claims submission process.
This guide is not intended to be an all-inclusive list of covered services under the Health Plan.
PRO_2909915E Internal Approved 02222024
©2024 Wellcare. All rights reserved. 2909915_MS4PCARGDEE

CLAIM SUBMISSION INFORMATION
SUBMISSION INQUIRIES:
Support from Provider Services: 1-855-538-0454
For inquiries related to your electronic or paper submissions to Wellcare, please contact our EDI team at [email protected].
ELECTRONIC FUNDS TRANSFER AND ELECTRONIC REMITTANCE ADVICE:
Register online using the simplified, enhanced provider registration process at payspanhealth.com or call 1-877-331-7154.
For more details on PaySpan, please refer to your Provider Manual.
CLEARINGHOUSE CONNECTIVITY:
Wellcare has partnered with Availity as our preferred EDI Clearinghouse. You may connect directly to Availity or continue to use
your existing vendor/biller/clearinghouse. If you need assistance in making a connection with Availity or have any questions,
please contact Availity client services at 1-800-282-4548.
FREE DIRECT DATA ENTRY DDE
Availity Essentials offers providers a web portal for direct data entry (DDE) claims that will submit to Wellcare electronically at
no cost to you. To register, submit the request to availity.com/Essentials-Portal-Registration.
PAYER IDs
• Fee-for-Service (FFS) is defined in the Transaction
Type Code BHT06 as CH, which means Chargeable,
expecting adjudication.
• Encounters (ENC) is defined in the Transaction
Type Code BHT06 as RP, which means
Reportable only, NOT expecting adjudication.
Claim Type
FFS
(CH – Chargeable)
Submissions
Encounter
(RF – Reporting only)
Submissions
Professional
or
Institutional
14163 59354
Visit our Claims page to locate claim forms and guidelines.
Wellcare does not accept handwritten, faxed or replicated claim forms. Wellcare does not accept media storage
devices such as CDs, DVDs, USB storage devices or flash drives.
MAIL PAPER CLAIM SUBMISSIONS TO:
Wellcare
Attn: Claims Department
P.O. Box 31372
Tampa, FL 33631-3372
CLAIM PAYMENT DISPUTES
The Claim Payment Dispute Process is designed to address claim denials for issues related to untimely filing, unlisted procedure
codes, non-covered codes etc. Examples include Explanation of Payment Codes DN001, DN038, DN039, VSTEX, HRM16 and
KYREC. However, this is not an all-encompassing list of Appeals codes. Claim payment disputes must be submitted in writing to
Wellcare within 90 calendar days of the date on the EOP.
Submit all claims payment disputes with supporting documentation at provider.wellcare.com or by mail.
NOTE: Wellcare does not accept media storage devices such as CDs, DVDs, USB storage devices or flash drives.
CLAIM PAYMENT DISPUTES WITH
SUPPORTING DOCUMENTATION MAY
ALSO BE MAILED TO:
Wellcare
Attn: Claim Payment Disputes
P.O. Box 31370
Tampa, FL 33631-3370
Fax: 1-877-277-1808
Note: Any appeals related to a claim denial for lack of prior authorization, services exceeding the authorization,
insufficient supporting documentation or late notification must be sent to the Appeals (Medical) address in the
section below. Anything else related to authorization or medical necessity that is in question should be sent
to the Appeals P.O. Box. Include all substantiating information (please do not include image of claim) like a
summary of the appeal, relevant medical records and member-specific information.
Page 2 of 11

CLAIM PAYMENT POLICY DISPUTES
The Claims Payment Policy Department has created a new mailbox for provider issues related strictly to payment policy issues.
Disputes for payment policy-related issues must be submitted to us in writing within 90 calendar days of the date on the EOP
(refer to your contract for required timing). Please provide all relevant documentation (please do not include image of Claim),
which may include medical records, in order to facilitate the review.
Submit all Claims Payment Policy Disputes related to Explanation of Payment Codes beginning with IH###,
CE###, CV### (Medical records required) or PD### at provider.wellcare.com or by mail.
NOTE: Wellcare does not accept media storage devices such as CDs, DVDs, USB storage devices or flash drives.
IH###, CE###, CV###
MEDICAL RECORDS REQUIRED
OR PD### TO:
Wellcare
Attn: Payment Policy Disputes Department
P.O. Box 31426
Tampa, FL 33631-3426
CPI## 1ST LEVEL INCLUDE ALL
MEDICAL RECORDS AND INITIAL
REVIEWS APPEALS TO:
BY MAIL U.S. POSTAL SERVICE
Optum
P.O. Box 52846
Philadelphia, PA 19115
Phone: 1-844-458-6739 | Fax: 1-267-687-0994
BY DELIVERY SERVICES FEDEX, UPS
Optum
458 Pike Road
Huntingdon Valley, PA 19006
BY SECURE INTERNET UPLOAD
Refer to Optum’s Medical Record Request letter
for further instructions.
LT###, RVLT# AND CPI##
2ND LEVEL APPEALS TO:
Wellcare
Attn: CCR
P.O. Box 31394
Tampa, FL 33631-3394
RVPI# TO:
PICRA
P.O. Box 31416
Tampa, FL 33631-3416
Page 3 of 11

RECOVERYCOST CONTAINMENT UNIT CCU
REFUND(S) in response to a Wellcare
overpayment notification should include
a copy of the overpayment notification as
well as a copy of attachment(s) and sent to:
Wellcare – Comprehensive Health Management
Attn: Recovery/Cost Containment Unit (CCU)
PO Box 947945
Atlanta, GA 30394-7945
NOTE: Wellcare does not accept media storage devices such as CDs, DVDs, USB storage devices or flash drives.
If you do not agree with this proposed Wellcare overpayment notification related to adjustments RVXX (Except RV059,
which should refer to the Claim Payment Disputes section above), you may request an Administrative Review by submitting
a dispute in writing within 45 days of the recovery letter date. Your request should detail why you disagree with these findings
and must include any supporting evidence/documentation you believe is pertinent to your position.
MAIL OR FAX YOUR ADMINISTRATIVE
REVIEW REQUEST TO:
Wellcare
Attn: CCU Recovery
P.O. Box 31658
Tampa, FL 33631-3658
Fax: 1-813-283-3284
Additional documentation received aft
er your initial Administrative Review request will not be considered. A Final Determination
will be rendered within 30 days of the date of Wellcare’s receipt of your request. If you do not submit a dispute or render payment
within the time period referenced above, we will take action to recover the amount owed as allowed by law, or as outlined within
the contract between you and Wellcare.
ADMINISTRATIVE REVIEWS RELATED TO EXPLANATION OF PAYMENT CODES AND COMMENTS BEGINNING
WITH DN227, DN228 OR RV213
must be submitted in writing and include at a minimum: a summary of the review request, the
member’s name, member’s identification number, date(s) of service, reason(s) why the denial should be reversed, copies of related
documentation and all applicable medical records related to both stays to support appropriateness of the services rendered.
YOUR DISPUTE SHOULD BE SENT TO:
Cotiviti
Attn: Wellcare Clinical Chart Validation
HillCrest III Building
731 Arbor Way, Suite 150
Blue Bell, PA 19422
Fax: 1-203-202-6607
Phone: 1-203-202-6107 (Inquiries Only)
PROVIDER-IDENTIFIED REFUND(S)
without receiving overpayment notification
should include the reason for overpayment
as well as any details that assist in identifying
the member and Wellcare Claim ID.
Wellcare – Comprehensive Health Management
Attn: Recovery/Cost Containment Unit (CCU)
PO Box 947945
Atlanta, GA 30394-7945
NOTE: For single-claim checks, please use the Refund Check Informational Sheet to help Recovery post accurately and
timely. For checks in excess of 25 claims, please complete the Refund Referral Grid and email all supporting documentation,
including the grid, to [email protected] to assist with expedited posting. Please note that only check
referrals will be accepted by this email box; anything other than check referrals will not be responded to and will be closed.
Page 4 of 11

APPEALS AND RECONSIDERATIONS MEDICAL
APPEALS NONPARTICIPATING PROVIDERS AND MEMBERS: Procedures that deal with the review of adverse initial
determinations made by the plan on health care services or benefits under Part C or D the enrollee believes they are entitled
to receive.
RECONSIDERATIONS PARTICIPATING PROVIDERS: A reconsideration is the first appeals process level. Reconsiderations
involved an MA plan reviewing an adverse organization determination, the findings they based them on, along with other evidence.
All non-participating Medicare provider appeals must be submitted within 60 calendar days from the date of the notice
of the initial determination and they must also submit a signed waiver of liability (WOL) with their request for processing.
Accompanying the WOL, an Appointment of Representative form is needed for the WOL process whenever a vendor (such
as a billing entity) is appealing on behalf of a non-participating provider. When submitting an appeal, the specific code or
service being appealed must be listed on the appeal form. Anything else related to authorization or medical necessity that is in
question should be sent to the Appeals P.O. Box. Include all substantiating information (please do not include image of claim)
like a summary of the appeal, relevant medical records and member-specific information.
Participating providers must seek a reconsideration through the Appeals Department within 90 calendar days (required
timing is listed in your contract) of a claim denial for lack of prior authorization, services exceeding the authorization, insufficient
supporting documentation or late notification. When submitting a reconsideration, the specific code or service being reconsidered
must be listed on the appeal form. Anything else related to authorization or medical necessity that is in question should be sent to
the Appeals P.O. Box. Include all substantiating information (please do not include image of claim) like a summary of the appeal,
relevant medical records and member-specific information.
APPOINTMENT OF REPRESENTATIVE AOR: With the Member’s written consent, an appeal for denial of an authorization
for medical service/Part B Drug can be filed on the Member’s behalf by a participating Physician who has or is currently treating
the Member. If the Member wishes to use a representative, they must complete a Medicare AOR form, and the Member and
representative must sign the AOR form.
Non-Physician (Practitioner): Per CMS and the Social Security Act, a non-physician is not a qualified physician (e.g.).
Type of Practitioner* AOR Needed No AOR Needed
Certified Nurse Midwife (CNM) X
Certified Registered Nurse Anesthetist (CRNA) X
Clinical Nurse Specialist (CNS) X
Surgeon Assistant X
Anesthesiology Assistant X
Audiologist X
Licensed Clinical Social Worker (LCSW) X
Clinical Psychologist X
Non-Clinical Psychologist X
PT, OT, Speech Pathologist X
Registered Dietician or Nutrition Professional X
Advanced Registered Nurse Practitioner (ARNP) X
Nurse Practitioner (NP) X
Physician Assistant (PA) X
Page 5 of 11

APPEALS AND RECONSIDERATIONS MEDICAL CONTINUED
Physician: A person skilled in the art of healing; specifically, one educated, clinically experienced, and licensed to practice
medicine as usually distinguished from surgery. A person licensed to practice medicine; a medical director (e.g.).
Type of Physician* AOR Needed No AOR Needed
Doctor of Medicine (MD) X
Doctor of Osteopathic Medicine (DO) X
Doctor of Dental Surgery (DDS) or Dental Medicine (DMD) X
Doctor of Optometry (OD) X
Doctors of Obstetrics and Gynecology (OB-GYN) X
Chiropractor (Doctor of Chiropractor) X
Psychiatrist X
Provider: Any physician, hospital, facility, or other Health Care Professional who is licensed or otherwise authorized to provide
Health Care services in the State or jurisdiction in which they are furnished.
Type of Facility* AOR Needed No AOR Needed
Inpatient X
Behavioral Inpatient X
Home Health Agency X
Skilled Nursing Facility on own behalf X
Skilled Nursing Facility (PT, OT & ST) X
Physician Group on own behalf X
Physician Group (PT, OT & ST) X
Rehabilitation Facility (i.e., LTAC) X
Durable Medical Equipment X
*The above lists of Non-Physicians, Physicians and Providers is not intended to be an all-inclusive list, they are the most common
identified on an appeal.
NOTE: For both Appeals and Reconsiderations, Wellcare does not accept media storage devices such as CDs, DVDs,
USB storage devices or flash drives.
MAIL OR FAX ALL MEDICAL APPEALS
AND RECONSIDERATIONS WITH
SUPPORTING DOCUMENTATION TO:
Wellcare
Attn: Appeals Department
P.O. Box 31368
Tampa, FL 33631-3368
Fax: 1-866-201-0657
GRIEVANCES
Member grievances may be filed verbally by contacting Customer Service or submitted in writing via mail, email or fax.
Providers may also file a grievance on behalf of the member with the member’s written consent, AOR forms are available here.
NOTE: Wellcare does not accept media storage devices such as CDs, DVDs, USB storage devices or flash drives.
MAIL, EMAIL OR FAX ALL MEMBER
GRIEVANCES TO:
Wellcare
Attn: Grievance Department
P.O. Box 31384
Tampa, FL 33631-3384
Fax: 1-866-388-1769
Email: Please visit the Contact Us page on the website.
Page 6 of 11

PHARMACY SERVICES
PHARMACY SERVICES: 1-866-799-5318
Including after-hours and weekends
Rx BIN Rx PCN Rx GRP
610014 MEDDPRIME 2FFA
610014 MAC 2FHU (MA Only)
MAIL ORDER:
Click here to locate Express Scripts
®
Mail Order info:
Phone: 1-833-750-0201 (TTY: 711)
24 hours a day, 7 days a week
SPECIALTY PHARMACY:
AcariaHealth™
AcariaHealth is a national comprehensive specialty
pharmacy focused on improving care and outcomes
for patients living with complex and chronic conditions.
AcariaHealth is comprised of dedicated healthcare
professionals who work closely with physician offices,
including support with referral and prior authorization
processes. This collaboration allows our patients to
receive the medicine they need as fast as possible.
Representatives are available from Monday–Thursday,
8 a.m. to 7 p.m., and Friday, 8 a.m. to 6 p.m. ET.
AcariaHealth™ Pharmacy #26, Inc.
8715 Henderson Rd.
Tampa, FL 33634
Phone: 1-866-458-9246 (TTY: 1-855-516-5636)
Fax: 1-866-458-9245
Website: acariahealth.com
MEDICATION APPEALS: Fax: 1-866-388-1766
Click here to locate Medication Appeal Request (form)
and mail with supporting documentation to:
Wellcare
Attn: Pharmacy Appeals Department
P.O. Box 31383
Tampa, FL 33631-3383
Medication appeals may also be initiated by contacting
Provider Services. Please note that all appeals filed verbally
also require a signed, written appeal.
NOTE: Wellcare does not accept media storage devices
such as CDs, DVDs, USB storage devices or flash drives.
COVERAGE DETERMINATION REQUESTS:
Fax: 1-866-388-1767
Electronic Prior Authorization (ePA):
account.covermymeds.com
Click here to locate Coverage Determination Request
(form) to be submitted for the exceptions listed below:
• Medications not listed on the formulary
• Drugs listed on the formulary with a prior authorization (PA)
• Duplication of therapy
• Prescriptions that exceed the FDA daily or formulary
quantity limit (QL)
• Most self-injectable and infusion medications (including
chemotherapy administered in a physician’s office)
• Drugs that have a step edit (ST) and the first-line therapy
is inappropriate
• Drugs that have an age limit (AL)
• Drugs listed on the formulary with a quantity limit (QL)
Click here to locate the Medication Guide/Formulary
Click here to locate Pharmacy Request forms such as
Injectable Infusion, Express Scripts Mail Order Service, etc.
New Century Health (NCH) will manage Medical
Oncology Services.
New Century Health
Phone: 1-888-999-7713, Option 1
FOR HOME INFUSIONENTERAL SERVICES:
Once Authorization Approval is obtained through
Wellcare, if required, please contact our providers
below to initiate services:
Coram
®
:
Phone: 1-800-423-1411
Fax: 1-866-462-6726
Option Care Health™ aka Option Care
and BioScrip Infusion Services
®
:
Phone: 1-833-466-0358
Page 7 of 11

PRIOR AUTHORIZATION PA LIST
PRIOR AUTHORIZATION PA REQUIREMENTS
Use the Pre-Auth Needed tool on our website to determine if prior authorization is required. This Prior Authorization list is
provided as a quick reference. Most current information can be found within the Pre-Auth tool.
For fastest results, submit requests online at our website. If the procedure requested meets clinical criteria, the Web provides
an approval that can be printed for easy reference. The health plan supports the concept of the Primary Care Physician (PCP) as
the “medical home” for its members.
For members enrolled in a PPO plan, authorization is not required for non-participating providers and facilities,
however, services on the medical necessity/authorization required list below must be covered services within the
benefit plan and considered medically necessary for the plan to pay a portion of the out-of-network claim.
For members enrolled in a non-PPO plan, all services rendered by non-participating providers and facilities require
authorization, including requests to use the member’s Point-of-Service benefits. Specialists must coordinate all services
with the member’s PCP. It is the responsibility of the provider rendering care to verify that the authorization request has been
approved before services are rendered.
Urgent Authorization Requests and Admission Notifications: Call 1-855-538-0454 and follow the prompts.
• Notification is required for Inpatient Hospital admissions by the next business day (except normal maternity delivery
admissions). Phone authorizations must be followed by a fax submission of clinical information.
• Standard authorization requests may be submitted online or via fax to the numbers listed on the associated forms located here.
BEHAVIORAL HEALTH SERVICES
SECURE PROVIDER PORTAL
For Urgent and Inpatient Hospitalization Authorizations and Provider Services Phone: 1-855-538-0454
Please log in to submit your Outpatient Authorization Requests and Inpatient Clinical Submissions.
To obtain authorization, notification of an Inpatient admission is required on the next business day
following admission.
• Inpatient concurrent review is generally done by phone, but a fax option is available and the forms and fax numbers
can be found here.
• Psychological testing requests are to be submitted via fax. All other levels of care requiring authorization, including
outpatient services, may be submitted online.
Procedures and Services Auth Required Comments
Emergency Behavioral Health Services No
Non-contracted (non-participating)
Provider Services
Yes All services from non-participating providers
require prior authorization.
*Excluding members enrolled in a PPO plan
Behavioral Health Services See Comments Please refer to the Behavioral Health
Authorization List under Other Resources
for authorization requirements.
EMERGENCY SERVICES
Emergency Services for the following procedures and service do NOT require prior authorization:
• Emergency Behavioral Health Services
• Emergency Care Services
• Emergency Transportation Services
(excluding Air & Water Ambulances)
• Urgent Care Services
Page 8 of 11

CARDIOLOGY MANAGEMENT PROGRAM
Wellcare has partnered with New Century Health (NCH) to implement a new cardiology prior authorization program, the
Cardiology Management Program. This program is intended to help providers easily and effectively deliver quality patient
care. Effective October 1, 2023, cardiology services rendered in a physician’s office, in an outpatient hospital ambulatory
setting, or in an inpatient setting (planned professional services only) must be submitted to NCH for prior authorization. This
requirement applies to all of your Medicare members ages 18 and older.
Approvals issued by Wellcare before October 1, 2023, are effective until the authorization end date, but all prior authorization
requests needed after October 1, 2023, must be submitted to NCH.
Prior authorization can be requested by:
• Visiting NCH’s web portal at my.newcenturyhealth.com.
• Calling 1-888-999-7713, Option 1 (Monday through Friday, from 5 a.m. to 5 p.m., Pacific time).
INPATIENT SERVICES & DISCHARGE PLANNING
SECURE PROVIDER PORTAL
Please log in to submit your Authorization Requests & Inpatient Clinical Submissions.
To fax a request, please access our forms here.
Discharge planning requests for Home Health and DME should be submitted separately
using one of the methods outlined above.
Procedures and Services Auth Required Comments
Elective Inpatient Procedures Yes Clinical updates required for continued length of stay (LOS).
Hospice Yes
Inpatient Hospital Admissions Yes Clinical updates required for continued length of stay (LOS).
Long-Term Acute Care Hospital
(LTACH) Admissions
Yes
Contact CareCentrix for authorization:
Phone: 1-888-571-6028
Observations Yes
Elective procedures that convert to an Observation stay are
subject to outpatient authorization requirements.
Authorization Lookup Tool
Services performed during an urgent or emergent
Observation stay, such as Advanced Radiology or Cardiology,
do not require authorization.
Clinical updates required for continued length of stay (LOS).
Orthopedic Surgery Yes Contact National Imaging Associates for prior authorization:
Phone: 1-800-424-5388
Rehabilitation Facility
Admissions
Yes
Contact CareCentrix for authorization:
Phone: 1-888-571-6028
Skilled Nursing Facility
Admissions
Yes
Contact CareCentrix for authorization:
Phone: 1-888-571-6028
Spinal Surgery Yes
Contact National Imaging Associates for prior authorization:
Phone: 1-800-424-5388
Page 9 of 11

OUTPATIENT SERVICES & DISCHARGE PLANNING
SECURE PROVIDER PORTAL
Please log in to submit your Outpatient Authorization Requests & Clinical Submissions.
To fax a request, please access our forms here.
Pharmacy Medical Requests Fax: 1-888-871-0564
Discharge planning requests for Home Health and DME should be submitted separately
using one of the methods outlined above.
Procedures and Services Auth Required Comments
Select Outpatient Procedures Yes Please refer to the Authorization Lookup Tool for prior
authorization requirements.
Advanced Radiology Services:
CT, CTA, MRA, MRI, Nuclear
Cardiology, Nuclear Medicine,
PET & SPECT Scans
Yes
Contact National Imaging Associates for prior authorization:
Phone: 1-800-424-5388
Advanced Imaging Solution
Cardiology Services:
Cardiac Imaging, Cardiac
Catheterization, Diagnostic
Cardiac Procedures and
Echo Stress Tests
Yes Contact National Imaging Associates for prior authorization:
Phone: 1-800-424-5388
Cardiac Solution
Dialysis No
Durable Medical Equipment
Purchases and Rentals
Yes
Please refer to the Authorization Lookup Tool for prior
authorization requirements.
*For Home Infusion/Enteral Services, please refer to
the Pharmacy section above for the preferred provider
if the authorization is required.
Hospice Care Services No
Investigational & Experimental
Procedures and Treatment
Yes Refer to Clinical Coverage Guidelines
Secure Provider Portal
Laboratory Management
(Certain Molecular and
Genetic Tests)
Yes
Contact eviCore for authorization:
Phone: 1-888-333-8641
Wellcare Lab Management Program Criteria
Molecular and Genetic Testing Quick Reference Guide
Medical Oncology Services Yes
Contact New Century Health for authorization:
Phone: 1-888-999-7713, Option 1
Medical Oncology Program Services
Non-contracted
(non-participating)
Provider Services
Yes All services from non-participating providers require
prior authorization.
Orthopedic Surgery Yes
Contact National Imaging Associates for prior authorization:
Phone: 1-800-424-5388
Page 10 of 11
OUTPATIENT SERVICES & DISCHARGE PLANNING CONTINUED
Procedures and Services Auth Required Comments
Orthotics and Prosthetics Yes Please refer to the Authorization Lookup Tool for prior
authorization requirements.
Pain Management Treatment
(Certain Pain Management
Treatments)
Yes Contact National Imaging Associates for prior authorization:
Phone: 1-800-424-5388
Interventional Pain Management Solution
Physical and Occupational
Therapy (including home-
based therapy)
*Excluding Episode of
Care Requests.
Please contact Wellcare for
all services rendered during
an Episode of Care
Yes
Contact National Imaging Associates for prior authorization:
Phone: 1-800-424-5388
Physical Medicine Solution
Radiation Therapy Management Yes
Contact New Century Health for authorization:
Phone: 1-888-999-7713, Option 1
Radiation Therapy Management Program Resources
Sleep Diagnostics Yes
Contact eviCore for authorization:
Phone: 1-888-333-8641
Sleep Diagnostics Program Criteria
Sleep Management Worksheets
Speech Therapy Yes
Contact National Imaging Associates for prior authorization:
Phone: 1-800-424-5388
Spinal Surgery Yes
Contact National Imaging Associates for prior authorization:
Phone: 1-800-424-5388
Transplant Services Yes Please submit clinical records for prior authorization for all
transplant phases.
Wound Care See Comments For CPT’s 11004, 11005, 11008, 11011, 11012, 11042, 11043,
11044, 11045, 11046 and 11047 No authorization is required
for the first 12 visits. After 12 combined visits or paid claims,
authorization would be required.
Page 11 of 11
