Pasco County Schools
Your 2023 Voluntary Reference Guide
Kurt S. Browning, Superintendent

Pasco County Schools: Table of Contents
It’s time to rock enroll.
Table of Contents
Dental 1
Vision 4
Flexible Spending Account 8
Supplemental Term Life Insurance 10
Disability Benefits 14
Additional Benefits 16
• Accident 18
• Cancer 23
• Critical Illness 28
• Hospital Indemnity 33
• Term to 100 Life Insurance 38
Legal with Identity Theft Protection 42
Electronic Device Protection Program 44

Pasco County Schools: Dental Benefits
Dental Benefits
Provider: Delta Dental
Voluntary dental plans are available to all benefit
eligible employees and their eligible dependents.
What Dental Plans are available?
Pasco Schools offer three dental plans for you to choose from:
• DHMO (Delta Care USA)
• PPO Low Plan
• PPO High Plan
What about the networks?
You will have access to a large network of Delta Dental general
dentists and specialty dentists. With enrollment in the PPO High or
Low plans, you have the freedom to choose to see an in-network or
out-of-network provider.
Delta Dental offers both the Delta Dental PPO and Delta Dental
Premier Networks. By selecting the Delta Dental PPO network, you
will usually achieve greater savings, due to lower negotiated fees.
Additionally in this plan you do have the option of using a dentist not
participating with Delta Dental; however you will need to file paper
claims and it usually results in higher out-of-pocket cost to the member.
If you choose to participate in the DHMO Plan you will have to select
a participating dentist from the DeltaCare USA network. In order to be
covered for services under the DHMO plan, you must have services
provided at your selected DHMO dental office. You can access the
network directories of participating dentists by visiting
deltadentalins.com.
1

2
Pasco County Schools: Dental Benefit
Is there an age limitation for children to see a pediatric dentist?
If you are enrolled in the DHMO plan, your primary dental office must refer your child (under 8 years of age) to a pediatric
dentist. If you are enrolled in the PPO plan- there are no age limits that are applicable.
If you are traveling and experience a dental emergency, please contact Delta Dental customer service and a representative
will assist you with treatment options.
What is a diagnostic & preventive maximum waiver (D&P waiver)?
Your PPO plans includes a D&P Maximum Waiver benefit, allowing you to obtain diagnostic and preventive dental services
without those costs applying towards the plan year maximum. This benefit promotes good oral health and may reduce the
need for more expensive, restorative dental services that can result from undetected oral or related health problems.
Which plans oer an orthodontic benefit?
The DHMO and the PPO High plans offer orthodontic coverage.
Who’s eligible?
Primary enrolled employee, spouse, eligible dependent children to age 26. Coverage will end at the end of the month in
which a dependent child reaches age 26 (unless that dependent child is disabled.)
What is a pre-authorization?
We do encourage you to have your dentist submit a preauthorization request for a reatment plan that will cost more than
$300. This will ensure that any of the procedures your dentist suggests are, in fact, covered benefits. It also gives you a
chance to find out beforehand what your out-of-pocket expenses will be.
What if I need to see a specialist?
Specialists. The DHMO is a “direct referral” plan. This means your general dentist will refer
you to a contracted specialist in your area.
What if I would like a second opinion?
Just let DeltaCare know that you would like another clinical opinion and they will
provide the name of a dentist for you to see.
For more information regarding your dental benefit?
Go to the Employee Benefits Department website and follow the links to Delta Dental.
To locate an in-network provider please visit www.deltadentalins.com.
Do any of the dental plans have a pre-exisiting condition clause?
No. There are no pre-exisiting condition clauses associated with any of the dental plans.

Who’s Eligible:
Primary enrollee, spouse, eligible
dependent children to age 26
High PPO Plan Low PPO Plan DeltaCare USA DHMO
Dental Network In-Network Out-of-Network In-Network Out-of-Network In-Network Only
Dental Networks- Payment Basis PPO
Premier/MPA
PPO PPO 14A
Plan Year Maximum $1,500 per covered member $1,000 per covered member
No Plan Year Max for
covered members
Deductible (Per Member/
Per Family) Per Calendar Year
$75/$225 $75/$225 $75/$225 $75/$225 Office Visit $0 Co-Pay
Diagnostic & Preventive SVC (D&P) 100% 100% 100% 60% D&P $0-$70 Co-Pay
Deductible Waived for D&P Yes Yes Yes Yes N/A
Basic Service 80% 80% 80% 50% DeltaCare Schedule A
Major Services 50% 50% 50% 40% DeltaCare Schedule A
Orthodontics- 3 Treatment Levels
(applies to DHMO only)
50% Not Covered $1900 Child $2100 Adult
Lifetime Ortho Max $1,000 Not Covered N/A
Coverage Eligibility Child & Adult Not Covered Child & Adult
Simple Extractions Basic Basic Basic Basic DeltaCare Schedule A
Complex Oral Surgery Basic Basic Basic Basic DeltaCare Schedule A
Endodontics (Root Canal) Basic Basic Basic Basic DeltaCare Schedule A
Periodontics (Gum Disease) Basic Basic Basic Basic DeltaCare Schedule A
Crowns, Bridges, Inlays, Onlays Major Major Major Major DeltaCare Schedule A
Implants Major Major Not Covered Not Covered
Dental Benefits
Pasco County Schools: Dental Benefits
4
3
Delta Detal DHMO 14A PPO High Plan PPO Low Plan
24 Ded 20 Ded 24 Ded 20 Ded 24 Ded 20 Ded
Employee
Employee Emp
$9.75 $11.70 $22.04 $26.45 $14.72 $17.67
Employee + 1 Dependent $17.06 $20.48 $54.96 $65.95 $35.73 $42.88
EE+ 2 or more Dependents $26.82 $32.18 $75.23 $90.28 $49.88 $59.86
Dental Rates - per pay deductions

Vision Benefits
Provider: Davis Vision by MetLife
Vision coverage is available for Pasco County
employees and their dependents. The vision
plan covers routine eye examinations,
corrective lenses, frames and contact lenses.
What are the benefits?
Option 1 & 2 (one-pair benefit) plan frequencies:
• Exam every January 1st
• Lenses every January 1st
• Two frames every other January 1st
Option 3 (two pair benefit) plan frequencies:
• Exam every January 1st
• Lenses every January 1st
• Two frames every other January 1st
*Note: If you enroll in the vision program your initial enrollment period drives eligibility for your
frames. Whenever the member 1st uses the frame benefit after enrolling is when the frame
benefit frequency begins.
• Member A enrolls 2/15/2023. Member A first uses the frame benefit on 4/10/2023.
Member A is next eligible for frame benefit on 1/1/25.
• Member B enrolls 2/15/2023. Member B first uses the frame benefit on 1/30/2024.
Member B is next eligible for frame benefit on 1/1/26.
Are there any restrictions or limitations?
If you see a Davis Vision participating provider, you will receive full benefits. If you use a
non-participating provider, your benefits will be reduced..
Could I incur additional costs?
Yes, depending upon the plan option that you choose. If you choose option 2 or 3, you will see
in the comparison chart that extra features such as tint or polarized lenses will be covered
without any additional charges. Please refer to the coverage chart for more detail regarding
covered benefits and co-payment costs.
What is the out-of-network reimbursement schedule?
• Eye Examination up to $52 - Frame up to $45
• Spectacle Lenses (per pair) up to:
• Single Vision $55, Bifocal $75, Trifocal $95, Lenticular $95
• Elective Contacts up to $105, Medically Necessary Contacts up to $210
4
Pasco County Schools: Vision Benefits
833-Eye-Life (833-393-5433) or www.metlife.com/mybenefits

How do I receive services from a provider in the network?
• Call the network provider of your choice and schedule an appointment.
• Identify yourself as Davis Vision plan participant.
• Provide the office with the member’s ID number and the date of birth of any covered children needing
services. It’s that easy! The provider’s office will verify your eligibility for services, and no claim forms
or ID cards are required.
For additional information:
Beginning 1/1/2023, please call Metlife at 833-Eye-Life (833-393-5433) with questions or visit our website:
www.metlife.com/mybenefits.
Member Service Representatives are available: 8:00 a.m. to 9:00 p.m. EST Monday-Friday and
9:00 a.m. to 4:00 p.m. EST Saturday. Participants who use a TTY (Teletypewritter)
because of a hearing or speech disability may access TTY services by calling 833-Eye-Life (833-393-5433).
Effective 1/1/2023 the plan becomes Davis Vision by Metlife.Client Codes are no longer used post 1/1/2023.
833-Eye-Life 833-393-5433
metlife.com/mybenefits
Pasco County Schools: Vision Benefits
5
Davis Vision Rates 2023
Option 1: Designer 24 Pay 20 Pay
Employee Only $6.55 $7.86
Employee + One $11.78 $14.13
Family $18.32 $21.99
Option 2: Premier Platinum Plus 24 Pay 20 Pay
Employee Only $10.63 $12.75
Employee + One $19.13 $22.96
Family $29.76 $35.71
Option 3: Premier Platinum Plus 2 Pair 24 Pay 20 Pay
Employee Only $17.92 $21.51
Employee + One $32.26 $38.71
Family $50.18 $60.21
Vision Plans - per pay deductions

DV-MKG18-0293v001 PDF 10/2018
Services Frequency
Plan design options
Option I: Designer
CC#: 2825
Option II: Premier
platinum plus
CC#:2826
Option III: Premier
platinum plus
1
)
CC#: 2827
Eye examination
Includes dilation when professionally indicated
Every
12 months
$10 copayment $10 copayment $10 copayment
Frames
Retail allowance
Every
24 months
Up to $130
plus 20% discount
2
Up to $150
plus 20% discount
2
Up to $150
plus 20% discount
2
Davis Vision frame collection
(in lieu of allowance)
Fashion
Covered in full Covered in full Covered in full
Designer
Covered in full Covered in full Covered in full
Premier
$25 copayment Covered in full Covered in full
Spectacle lenses
Includes single-vision, bifocal, trifocal, lenticular,
polycarbonate lenses, and scratch-resistant & UV
coating, other lens options available
Every
12 months
$15 copayment
$15 copayment
includes most lens
options, Covered in full
$15 copayment
includes most lens
options, Covered in full
Contact lenses (in lieu of eyeglasses)
Retail allowance
Every
12 months
Up to $130
plus 15% discount
2
Up to $150
plus 15% discount
2
Up to $150
plus 15% discount
2
Davis Vision collection
(in lieu of allowance)
Covered in full Covered in full Covered in full
Visually required
Covered in full Covered in full Covered in full
Contact lens evaluation,
Fitting & follow-up care
Every
12 months
$15 copayment $15 copayment $15 copayment
Retail allowance: standard type
Covered in full Covered in full Covered in full
Retail allowance: specialty type
Up to $60
plus 15% discount
2
Up to $60
plus 15% discount
2
Up to $60
plus 15% discount
2
Davis Vision collection
Covered in full Covered in full Covered in full
Visually required
Covered in full Covered in full Covered in full
1
Members have three options available; two pairs of eyeglasses; one pair of eyeglasses & contact lenses; or two dispenses of contact lenses
2
Additional discounts not available at Walmart or Sam’s Club locations
Out-of-network reimbursement rate
Eye examination up to $52 | Frame up to $45
Spectacle lenses (per pair) up to:
Single vision $55, Bifocal $75, Trifocal $95, Lenticular $95
Elective contacts up to $105, Visually required contacts up to $210
Monthly Rates
Option I Option II Option III
Employee Only
$12.59 $19.68 $32.58
Employee + One
$22.64 $35.42 $58.64
Employee + Family
$35.23 $55.10 $91.23
Contact your bene昀ts
department today to enroll.
etietepanbeoeaiiionb
etieantenewponei-e-ie
--anwebiteetieobeneit
taeeetientoeare
noonerepot
Vssf
Pasco County School employees
Pasco County Schools: Vision Benefits
6
833-Eye-Life (833-393-5433) or www.metlife.com/mybenefits

DV-MKG18-0293v001 PDF 10/2018
Please call Davis Vision at 1 (800) 999-5431 with questions or visit our Web site: www.davisvision.com.
Member Service Representatives are available (EST): Monday through Friday, 8:00 AM to 11:00 PM, Saturday,
9:00 AM to 4:00 PM, and Sunday, 12:00 PM to 4:00 PM. Participants who use a TTY (Teletypewriter) because
of a hearing or speech disability may access TTY services by calling 1 (800) 523-2847.
Want additional information?
Spectacle lenses bene昀t
Plan design
Option I: Designer
CC#: 2825
Option II: Premier
platinum plus
CC#:2826
Option III: Premier
platinum plus
/1
)
CC#: 2827
All ranges of prescriptions and sizes Included Included Included
Choice of glass or plastic lenses Included Included Included
Tinting of plastic lenses Included Included Included
Scratch-resistant coating Included Included Included
Polycarbonate lenses Included Included Included
Ultraviolet coating Included Included Included
ddcvcg $35 Included Included
Premium AR coating $48 Included Included
Ultra AR coating $60 Included Included
Ultimate AR coating $85 $85 $85
Standard progressive lenses Included Included Included
Premium progressive lenses $40 Included Included
Ultra progressive lenses $90 $50 $50
Ultimate progressive lenses
$15$5$5
Intermediate-vision lenses $30 Included Included
Blended-segment lenses $20 Included Included
High-index lenses 1.67 $55 Included Included
High-index lenses 1.74 $120 $120 $120
Polarized lenses $75 Included Included
Photochromic glass lenses $20 Included Included
Plastic photosensitive lenses $65 Included Included
Scratch protection plan:
Single vision lenses | multifocal
$20 | $40 $20 | $40 $20 | $40
Value-added features:
Replacement contacts through DavisVisionContacts.com mail-order contact lens replacement service ensures easy,
convenient purchasing online and quick shipping direct to your door. Davis Vision provides you and your eligible dependents
with the opportunity to receive discounted laser vision correction, often referred to as LASIK. For more information, visit
www.davisvision.com.
How do I receive services from a provider in the network?
• Call the network provider of your choice and schedule an appointment.
• Identify yourself as Davis Vision plan participant.
• vdhchhmmsDumdhdfhfycvdchlddgsvcs.
shsyhvdscllvfyyulglyfsv
csdclmfmsDcdsud!
Who are the network providers?
They are licensed providers who are extensively reviewed and credentialed to ensure that stringent standards for quality
service are maintained. Please call 1 (800) 999-5431 to access the Interactive Voice Response (IVR) Unit, which will supply
you with the names and addresses of the network providers nearest you, or you may access our Web site at
www.davisvision.com and utilize our “Find a Doctor” feature.
7
Pasco County Schools: Vision Benefits

8
Pasco County Schools: Flexible Spending Accounts
Medical & Dependent Care Flexible Spending Accounts
Provider: WageWorks
Flexible Spending Accounts
Flexible Spending Accounts are optional benefit plans that allow you to
direct a part of your pay, TAX-FREE, into two accounts, described
below. A Healthcare Flexible Spending Account (HFSA) can be used to
pay for out-of-pocket medical expenses for you and your tax
dependents. These include charges for office visits, amounts toward
your deductible, prescriptions, dental work, eyeglasses, contacts
and lab fees. The Dependent Care Flexible Spending Account (DFSA)
can be used to pay for daycare or elder care expenses.
Your FSA deposits are not taxable income on your W-2. Since
your annual income is reduced, so are your annual taxes.
Medical FSA (Deductions occur 20 times per year)
How the FSA tax advantage works - Medical Flexible Spending
(MFSA)
First, determine your election amount: For the HFSA, the minimum is
$200 and the maximum is $2,850. Your election amount divided by the
number of paychecks that you receive during the plan year will tell you
what will be deducted pre-tax from each pay period.
You get the exclusive FSA debit card
The WageWorks FSA card can be used at any provider or merchant
classified as a medical, dental or vision provider. It is limited to doctor’s
offices, pharmacies, hospitals, dental providers, vision providers, and
medical labs.
Use of the card is optional. You can also use a different form of
payment and then submit the claim to WageWorks on their website
or via their mobile application.
When using the card, please be sure to keep all of your receipts.
You may be required to submit them to WageWorks.. The IRS
requires that you substantiate all charges. WageWorks will
attempt to do so systematically, but may contact you and request
a receipt for your card transactions.
Due to Health Care Reform, over-the-counter (OTC) medicines and
drugs, except for insulin, will require a letter of medical necessity or
prescription from your physician to be reimbursed from your medical
FSA. If you have any questions regarding whether a health-related
supply is eligible please contact WageWorks customer services.
WageWorks 877.924.3967 or visit www.wageworks.com

9
Pasco County Schools: Flexible Spending Accounts
How Do You File a Claim?
Your Flexible Spending Account (FSA) is offered by WageWorks.
With this you will have several conveniences:
• Fast and efficient claim reimbursements
• Multiple claim submission options including online, fax or
regular mail.
• Online account access 24 hours a day/ 7 days a week
• Toll-free customer service assistance, email and web chat
customer service
• Interactive Voice Response System availability 24 hours/ 7 days
a week to check account activity, account balance, and more
• Opportunity to sign up for text/ email notifications of
account activity
How do I avoid losing money?
Pasco Schools allows the “carry over” option that enables you to carry
over from one year to the next a maximum of $550 of unused funds.
If on December 31, you have an unused amount that exceeds the
$550 carry over, it will be forfeited. When making your election, please
consider what your expected out-of-pocket expenses will be for the
coming year for yourself and your tax dependents. The “Carry over”
amount will be available to use after your 2023 account balance
has been exhausted.
Please note that should your employment end during the plan year,
your eligibility ends as of the last day of the month of your termination,
yet you would still have ninety days to submit claims for dates-of-ser-
vice that fell on or before your termination date. Monies not claimed
within ninety days of your termination will be forfeited. Also, you are
not eligible for the carryover of funds unless you are an active partici-
pant on the last day of the plan year or if you extend your FSA via
COBRA thru the end of the year.
Dependent Care Reimbursement FSA Account
(Deductions occur 20 times per year)
A Dependent Care reimbursement account gives you the opportunity
to pay for the first $5,000 of employment-related dependent care
expenses, tax-free. Your eligible dependents are children under
the age of 13 and adults incapable of self-care that you claim as
dependents. The DFSA, the minimum is $200 and the maximum is
$5,000 (if married and filling jointly.) There is a maximumof $5,000 for
the household if it’s two married employees of the board.
What are eligible dependent care expenses?
• Expenses for services provided in your home as long as someone
you claim as a dependent, or other children under age 19 are not
providing these services.
• Expenses for daycare services outside your home at a facility
compliant with state and local laws.
• Dependent care expenses include adult daycare center, after
school program, babysitting (work-related), before and after school
programs, child care, custodial elder care (work-related), elder
care (while you work, to enable you to work or look for work),
senior daycare, and sick childcare.
Questions
Should you have any immediate questions, please contact WageWorks
Customer Service at 877-924-3967. You can also visit our website
at www.wageworks.com
Please note that should your employment end during the plan
year, your eligibility ends as of the last day of the month of
your termination, yet you would still have ninety days to submit
claims for dates-of-service that fell on or before your termination
date. Monies not claimed within ninety days of your termination
will be forfeited. Also, you are not eligible for the carryover of
funds unless you are an active participant on the last day of the
plan year or if you extend your FSA via COBRA thru the end of
the year.

10
Pasco County Schools: Supplemental Term Life Insurance
Basic Term Life Insurance
Pasco County Schools provides an employer-paid basic life
benefit to all benefit eligible employees through Minnesota Life.
You also automatically receive a matching amount of $35,000 of
Accidental Death and Dismemberment coverage as part of your basic
life insurance benefit. This benefit is provided at no cost to you.
Supplemental Life Insurance
In addition to the $35,000 basic term life insurance received, you may
purchase supplemental life insurance for yourself, your spouse and
your children. The supplemental life insurance is an age-banded
benefit; premium amounts are based on your age and the amount of
coverage that you select. During Open Enrollment coverage may
increase by $20,000 with no evidence of insurability required. Any
additional increase over $20,000 will require evidence of insurability
and medical underwriting. During open enrollment, you may increase
your existing supplemental life coverage by one or two $10,000
increments, up to a maximum of 5 times your annual salary or
$300,000, without answering health questions. To apply for coverage
other than what's outlined here, you'll answer three questions about
your health history - along with height and weight.
What is accidental death and dismemberment
(AD&D) insurance?
AD&D coverage is included in your basic life insurance benefit
provided by Pasco County Schools. AD&D means that when your
death or dismemberment results directly from an accidental injury
which is unintended, unexpected and unforeseen the policy pays a
benefit in addition to the basic life insurance benefit. The benefit
amount is equal to the amount of the basic life benefit. For example,
an employee would have $35,000 of AD&D Insurance in addition to
the $35,000 of Basic Life Insurance. There is not an AD&D benefit
associated with supplemental policies.
Employee Supplemental Life
You may purchase supplemental life insurance coverage for yourself
in $10,000 increments up to 5 times your salary or a maximum of
$300,000, whichever is less. If you enroll in coverage as a new benefit
eligible employee, you may apply for up to the maximum amount
of coverage that you are eligible for without having to answer health
questions.
Spouse Life Insurance
As a new employee, when you are first eligible for benefits, you may
purchase coverage in $5,000 increments, up to a maximum of
$25,000 for your spouse, without having to answer health questions.
Spouse supplemental life insurance can be purchased in $5,000
increments, not to exceed 100% of the employee’s coverage or
$150,000 (whichever is less). Any additional elections or increases in
coverage will require you to answer health questions.
If both spouses work for Pasco County Schools, an employee
cannot be covered by their spouse.
Do I need to complete an evidence
of insurability form?
Enrolling for coverage other than what is outlined on page one will
require that you answer three questions about your health history,
along with height and weight. Based on your answers, it will be deter-
mined whether anything further is needed to make a decision to
approve or decline the application. If by any chance your application is
not approved, you will still get any coverage that didn't require the
health questions and it will not affect any coverage you already have.
In the following situations, the life insurance carrier requires applicants
to complete a medical underwriting form (Medical History Statement)
regarding past health history: Evidence of Insurability (EOI) is
required:
• Employees not currently enrolled
• Employees enrolled in supplemental life insurance policy allows
for reinstatement within 1 year. See "Can your insurance be
reinstated after termination?" section on the certificate, who are
requesting an increase in coverage of more than $20,000
• Reinstatement of Benefits: Any request to reinstate a life
insurance benefit
Newly hired employees: Evidence of Insurability (EOI) -
Medical underwriting is not required.
Supplemental Term Life Insurance
Provider: Minnesota Life
Securian Financial lifebenefits.com

11
Pasco County Schools: Supplemental Term Life Insurance
Electronic Evidence of Insurability
Process (EOI)
If you recently elected to increase your group life insurance
coverage by more than $20,000 or you are enrolling for the
first time you must submit a satisfactory Evidence of Insurability
EOI). This year you may complete your EOI online.
Before you begin:
• The process will take 10-30 minutes to complete
• You will not be able to save your work to return later
• An email address is required
• Have your medical records available
• If you have elected spouse coverage, they must complete
their questions during the same session
• Visit www.LifeBenefits.com/SubmitEOI
• Provide your group policy number- 33290
• Enter your access key – pasco
• Complete the word validation
This electronic process is not available for “child”
supplemental life. A paper EOI form must be completed.
It can be obtained on-line in Munis on the page that
the benefit is elected (icon on top of page). Any
new coverage for children with the exception of
new hires will require an evidence of insurability
to be completed. A link to the paper form is
available during open enrollment.
Group policy number - 33290

12
Pasco County Schools: Supplemental Term Life Insurance
How do I designate a beneficiary?
To assign beneficiaries for your Life insurance policy (core and
supplemental), you must use your assigned log-in ID and
password sent to you by Minnesota Life in the mail to sign into
www.lifebenefits.com website to designate your beneficiaries.
You may assign multiple primary and contingent beneficiaries, as
long as the percentages are in whole numbers, and equal 100
percent. Contingent beneficiaries will only receive a benefit if none
of the primary beneficiaries survive you. You can change your
beneficiaries at any time by logging onto lifebenefits.com.
Age Reductions (Supplemental Life only)
Age reductions apply to supplemental life coverage only. Age
reductions will apply the first day of the month following and insured
employee’s 70th and 75th birthdays. The amount of supplemental
insurance on an employee age 70 or older shall be a percentage of
the amount otherwise provided by the plan of insurance. Age 70=65%
of the amount of insurance, Age 75=50% of the amount of insurance.
(Example: $100,000 of coverage reduces to $65,000 at age 70 and
$50,000 at age 75)
Are my life insurance benefits reduced while
I grow older?
Your basic core life insurance benefit ($35,000) does not reduce with
age for active employees. Supplemental policies will reduce with age.
See your certificate of coverage for information regarding benefit
reductions due to age.
Can I collect my life insurance benefit while I am
still living?
Both the Basic Employee Life policy and the supplemental employee
life insurance include an Accelerated Benefit that allows an insured
employee with a “Qualifying Medical Condition” to receive up to 75%
of the amount of the insured’s life insurance. A “Qualifying Medical
Condition” is a terminal illness or physical condition that is reasonably
expected to result in death within 12 months.
The receipt of this benefit may be taxable and may affect your
eligibility for Medicaid or other government benefits or entitlements,
so you should consult your tax or legal advisor before you apply for
an Accelerated Benefit.
How do I submit a claim?
If you need to submit a claim, please contact our Risk Management
at 813-794-2520.
Do I still need to pay my premium of coverage if I
become disabled?
The waiver of premium benefit is available for those who become
totally and permanently disabled prior to age 60. Contact Risk
Management to receive the waiver of Premium Application.
Supplemental Term Life Insurance
Provider: Minnesota Life
Securian Financial lifebenefits.com

13
Pasco County Schools: Supplemental Term Life Insurance
Can I take my life insurance with me if I leave
Pasco County Schools?
You are eligible to “port” (buy) your life coverage to take with you
when you leave employment with Pasco County Schools. This
portability option applies to basic and supplemental life policies. If you
are not in good health, you may be required to “convert” your basic
coverage which will result in a much higher premium amount due.
When you end your employment, you may visit the Employee Benefits
website and download the form to port your policy with
Minnesota Life. It will be your responsibility to download the portability
form and contact Minnesota life to continue your basic or
supplemental insurance benefit. This action must be taken within 60
days of your employment ending.
As part of your participation in this benefit, the following services are
available at no charge:
Travel Assistance
Services include a full range of medical, travel, legal and emergency
transportation services when you travel more than 100 miles from
home or internationally. Medical professional locator services,
assistance replacing lost or stolen luggage, medication, or other
critical items, medical or security evacuation.
Legal Services
You have access to an online library of legal forms, comprehensive
web and mobile resources. Also available is a free 30-minute
consultation with a participating attorney.
Legacy Planning
Access to a variety of information and resources to work through
end-of-life issues: End-of-life planning, final arrangements,
Express Assignment™ for expedited funeral home assignments.
Age
Employee Only
Per $10,000
Per Pay
Spouse Only
Per $5,000
Per Pay
Children Only
Per Pay
18-24 $0.29 $0.15 $0.79
25-29 $0.25 $0.12 —
30-34 $0.29 $0.15 —
35-39 $0.44 $0.22 —
40-44 $0.69 $0.35 —
45-49 $1.14 $0.57 —
50-54 $1.73 $0.86 —
55-59 $2.57 $1.28 —
60-64 $3.66 $1.83 —
65-69 $6.08 $3.04 —
70-74 $10.88 $5.44 —
75 & over $22.20 $11.10 —
Minnesota Life Rates
(Deductions occur 20 times per
year for all employees)
Securian Financial lifebenefits.com

14
Pasco County Schools: Long-Term Disability Benefits (LTD)
Long-Term Disability Benefits (LTD)
Provider: Unum
You may elect to participate in the Long-Term Disability benefit at
a per pay period cost to you. This coverage will pay you a monthly
benefit if you become disabled due to an accident or an illness and
are unable to work. In order to be eligible to receive a benefit,
an employee is required to exhaust all available sick time.
Please keep this in mind when choosing a benefit elimination
(waiting) period.
What is a waiting period?
The elimination period is the length of time you must be continuously
disabled before you can receive benefits. Employees have
the opportunity to choose which elimination (waiting) period fits their
needs. The options on elimination (waiting) periods are:
• 14 days for accident and 14 days for illness
• 30 days for accident and 30 days for illness
• 60 days for accident and 60 days for illness
• 90 days for accident and 90 days for illness
• 180 days for accident and 180 days for illness
What is the maximum dollar amount that
I can elect?
Coverage can be purchased in $100 increments up to a maximum of
60% of your annual salary, beginning at a minimum benefit selection of
$200. LTD premiums are paid by employees on a post-tax basis, so
the LTD benefits paid to employees are not taxed. When calculating
monthly benefits, it is important to note that your disability benefit may
be reduced by deductible sources of income and any earnings you
have while disabled. Deductible sources of income may include such
items as disability income or other amounts you receive or are entitled
to receive under: workers’ compensation or similar occupational benefit
laws; state compulsory benefit laws; automobile liability and no fault
insurance; legal judgments and settlements; certain retirement plans;
salary continuation or sick leave plans; other group or association
disability programs or insurance; and amounts you or your family
receive or are entitled to receive from Social Security or similar
governmental programs.
Unum Disability 800.635.5597
When am I considered disabled?
You are disabled when Unum determines that:
• You are limited from performing the material and substantial duties
of your regular occupation* due to sickness or injury; and
• You have a 20% or more loss of indexed monthly earnings due to
the same sickness or injury.
*After 24 months, you are disabled when Unum determines that due
to the same sickness or injury, you are unable to perform the duties
of any gainful occupation for which you are reasonably fitted by
education, training or experience
How long can LTD benefits continue?
There are two plan choices available:
Plan 1: Pays a monthly benefit up to age 65*.
Plan 2: Pays a monthly benefit for a maximum of 24 months.
*If a participant becomes disabled after age 60, benefits could extend
past age 65. Please refer to the certificate of coverage for the full
benefit duration schedule.There are two plan choices available:
Plan 1: Pays a monthly benefit up to age 65*.
Plan 2: Pays a monthly benefit for a maximum of 24 months.
*If a participant becomes disabled after age 60, benefits could extend
past age 65. Please refer to the certificate of coverage for the full
benefit duration schedule.

15
Pasco County Schools: Long-Term Disability Benefits (LTD)
How do I enroll?
Employees who would like to enroll in the LTD coverage must make
an election on the employee self-service portal. Please make sure to
select the plan details: the elimination (waiting) period, dollar amount
and benefit coverage duration.
Do I need to complete any special forms
to qualify?
Yes. Medical underwriting is required for any new coverage or
increase in coverage with the exception of new hires. An electronic
link will be provided to complete the EOI process.
• Please complete your Statement of Health (Evidence of Insurability)
• Access Code: 2LSY3TR
• You will need the following information before logging in to
complete your Statement of Health (Evidence of Insurability)
• Name, address, date of birth, social security number, gender,
employee annual salary, date of hire, phone number, and
email address
• Medical information such as height, weight, medical treatment
dates, duration, treatment received, medications and dosages,
names and addresses of physicians and hospitals
What is considered a pre-existing condition?
You have a pre-existing condition if:
• you received medical treatment, consultation, care or services
including diagnostic measures, or took prescribed drugs or
medicines in the 3 months just prior to your effective date of
coverage; and
• The disability begins in the first 12 months after your effective
date of coverage.
What if I have a pre-exisiting condition?
Pre-existing conditions apply to any added benefits or increases in
benefits or elimination periods. This limitation will not apply to a
period of disability that begins after the employee has been covered
for 12 months after the effective date of coverage, or the effective
date of any added or increased benefits.
I do not work over the summer. If I am disabled
in the summer can I collect a monthly benefit?
If your pay-type does not require you to work summer months, then
you will not receive a benefit during the summer months, when you
would not be missing scheduled work days.
This summary page provides a brief overview of your LTD Plan.
For a complete explanation of your coverage (exclusions, limitations
and reductions of your coverage) please refer to your Certificate
of Coverage.
How much can my monthly benefit be?
(Annual salary X 60%) /12 This calculation is rounded down
to the closest $100 increment. If you enrolled in a brand new
disability policy during Open Enrollment and you are not
present at work the first day back from winter break the
policy becomes null in void.

16
Pasco County Schools: Additional Coverage
Additional Coverage
You have the opportunity to buy additional coverage through
Allstate for life’s unexpected events.
Guaranteed issued:
• Accident
• Hospital
• Ter
m to Age 100
•
Critical Illness
• Cancer
Accident
Protection for accidental injuries that occur on or off the job. It includes
dislocations or fractures, hospital confinement, ambulance services and
more. You can select and individual or family plan.
Cancer
Receiving a cancer diagnosis can be one of life’s most frightening
events. With Cancer insurance you can rest a little easier. This
coverage pays you a cash benefit to help with the costs associated
with treatments, to pay for daily living expenses and more. You can
select and individual or family plan.
Hospital
The Hospital policy helps you pay for out-of-pocket medical expenses
associated with hospital confinements, other medical procedures
and/or visits. You can select and individual or family plan.
Critical Illness
Critical Illness coverage helps offer financial support if you are
diagnosed with a covered critical illness such as a heart attack, stroke,
and more. This plan also offers an additional wellness benefit for yearly
screenings such as mammogram, Colonoscopy, stress test and more.
New this year is an additional cancer benefit to Plan 1+ and Plan 2+.
You can select and individual or family plan.
Term to Age 100 Life Insurance
You choose the coverage that’s right for you and your family. Premiums
are affordable and remain level to age 100 unless you make changes.
Allstate 800.521.3535

Today, active lifestyles in or out of the home may result in bumps, bruises and
sometimes breaks. Getting the right treatment can be vital to recovery,
but it
can also be expensive. And if an accident keeps you away from work during
recovery, the financial worries can grow quickly.
Most major medical insurance plans only pay a portion of the bills. Our coverage
can help pick up where other insurance leaves off and provide cash to help cover
the expenses.
With Accident insurance from Allstate Benefits, you can gain the advantage of financial
support, thanks to the cash benefits paid directly to you. You also gain the financial
empowerment to seek the treatment needed to be on the mend.
Here’s How It Works
Our coverage pays you cash benefits that correspond with hospital and intensive
care confinement. Your plan may also include coverage for a variety of
occurrences,
such as: dismemberment; dislocation or fracture; ambulance services; physical therapy
and more. The cash benefits can be used to help pay for deductibles, treatment, rent
and more.
Meeting Your Needs
• Guaranteed Issue, meaning no medical questions to answer
• Benefits are paid directly to you unless otherwise assigned
• Pays in addition to other insurance coverage
• Coverage also available for your dependents
• Premiums are aordable and can be conveniently payroll deducted
•
Coverage can be continued; refer to your certificate for details
With Allstate Benefits, you can protect your finances against life’s slips and falls.
Are you in Good Hands? You can be.
Accident Insurance
Protection for accidental
injuries on- and off-the-job,
24 hours a day
Oered to the employees of:
Pasco County
Schools
ABJ30901X-1
*National Safety Council, Injury Facts®, 2017 Edition
DID YOU
KNOW
The number of injuries
suered
by workers in one year, both
on- and o-the-job, includes:*
?
ON-THE-JOB (in millions)
Work
4.4
OFF-THE-JOB (in millions)
Auto
2.2
Home
9.2
Non-Auto
4.0
17

Daniel’s story of injury and treatment turned into a happy ending,
because he had supplemental Accident Insurance to help with expenses.
Daniel was playing a pick-up game of basketball
with his friends when he went up for a jump-shot
and, on his way back down, twisted his foot and
ruptured his Achilles tendon
.
Here’s Daniel’s treatment path:
•
Taken by ambulance to the emergency room
• Examined by a doctor and X-rays were taken
• Underwent surgery to reattach the tendon
• Was visited by his doctor and
released after a
one-day stay in the hospital
• Had to immobilize his ankle for 6 weeks
• Was
seen by the
doctor during a follow-up visit
and sent to physical therapy to strengthen his
leg and improve his mobility
Daniel would go online after each of his treatments
to
file claims. The cash benefits were direct deposited
into his bank account.
Daniel is back playing basketball and enjoying life.
CHOOSE CLAIMUSE
Daniel and Sandy choose
benefits to help
protect their
family if they suffer an
accidental injury.
Meet Daniel & Sandy
Daniel and Sandy are like most active couples:
they enjoy the outdoors and a great adventure.
They have seen their share of bumps, bruises
and breaks. Sandy knows an accidental injury
could happen to either of them. Most
importantly,
she
worries about how they
will pay for it.
Here is what weighs heavily on her mind:
• Major medical will only pay a portion
of the expenses associated with injury
treatments
• They have copays they are responsible
for until they meet their deductible
• If they miss work because of an injury,
they must cover the bills, rent/mortgage,
groceries and their child’s education
• If they need to seek treatment not
available locally, they will have
to pay for it
Ambulance Services
Medicine
Medical Expenses
(Emergency Room and X-rays)
Initial Hospital Confinement
Hospital Confinement
Tendon Surgery
General Anesthesia
Accident Follow-Up Treatment
Physical Therapy (3 days/week)
For a listing of benefits and benefit
amounts, see your company’s
rate insert.
Daniel’s Accident claim paid cash
benefits for the following:

Benefits (subject to maximums as listed on the attached rate insert)
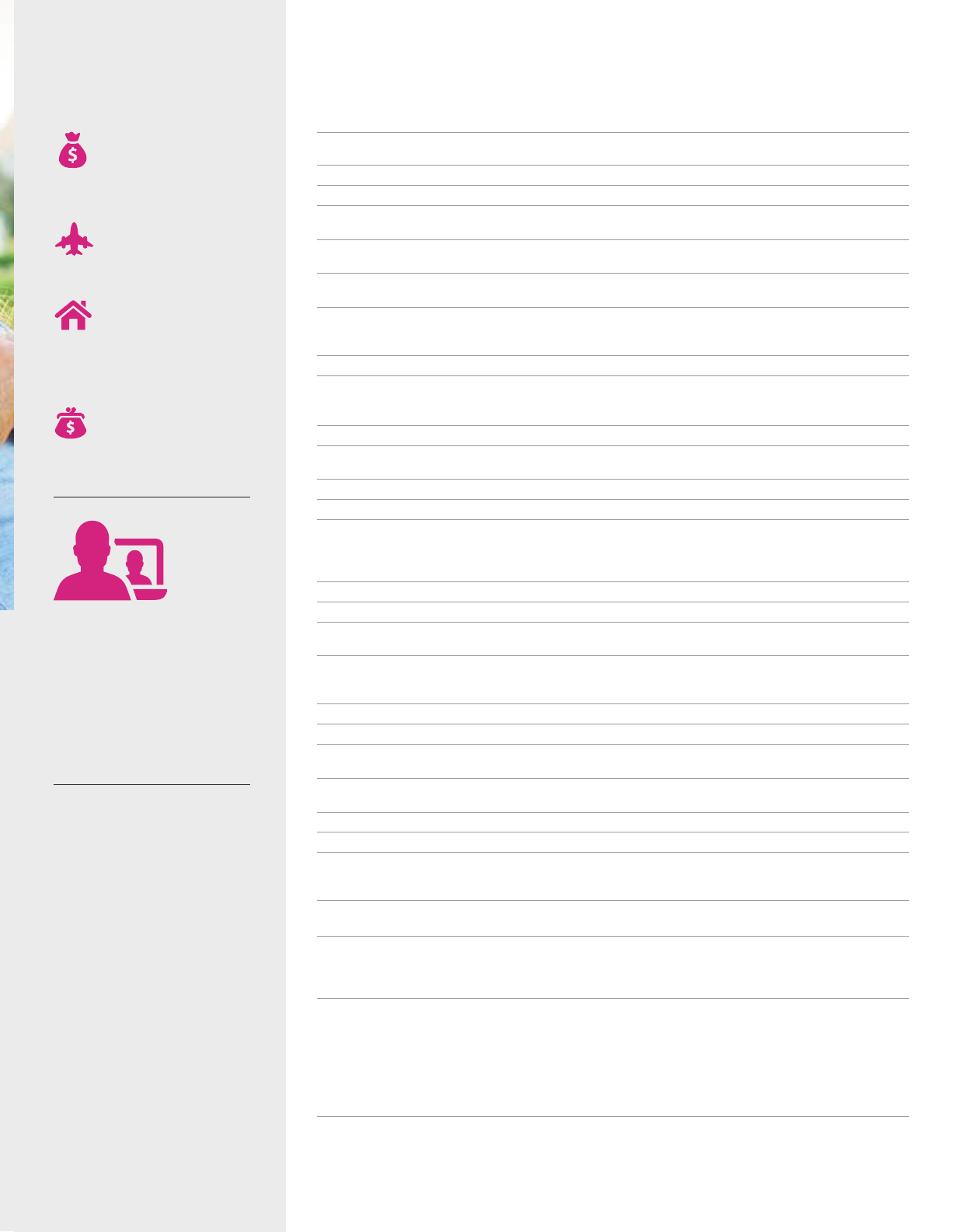
Using your cash benefits
Cash benefits provide you with
options, because you decide
how to use them.
Finances
Can help protect HSAs,
savings, retirement
plans and 401(k)s
from being depleted.
Trave l
Can help pay for expenses
while
receiving treatment
in another city.
Home
Can help pay the
mortgage, continue
rental payments, or
perform needed
home
repairs for after care.
Expenses
Can help pay your family’s
living expenses such as
bills, electricity, and gas.
An easy-to-use website that
offers 24/7 access to important
information
about your benefits.
Plus, you can submit
and check
your claims (including claim
history), request your cash
benefit to be direct deposited,
make changes to personal
information, and more.
Dependent Eligibility
Coverage may include you, your
spouse or domestic partner, and
your children.
1
Multiple dismemberments, dislocations
or fractures are limited to the amount
shown in the rate insert.
2
Up to three
times per covered person, per accident.
3
Two or more surgeries done at the
same time are considered one operation.
4
Paid for each day a room charge is
incurred, up to 30 days for each covered
person per continuous period of
rehabilitation unit confinement, for a
maximum of 60 days per calendar year.
5
Two treatments per covered person, per
accident. *Must begin or be received
within 180 days of the accident. **Within
3 days after the accident.
MyBenefits: 24/7 Access
allstatebenefits.com/mybenefits
BASE POLICY BENEFITS
Accidental Death
*
Common Carrier Accidental Death - riding as a fare-paying passenger on a scheduled common-carrier
Dismemberment
1,
*
-
amount paid depends on type of dismemberment. See Injury Benefit Schedule in rate insert
Dislocation or Fracture
1
-
amount paid depends on type of dislocation or fracture. See Injury Benefit Schedule in
rate insert
Initial Hospitalization Confinement -
initial hospitalization after the eective date
Hospital Confinement -
up to 90 days for any one injury
Intensive Care -
up to 90 days for each period of continuous confinement
Ambulance Services - transfer to or from hospital by ambulance service
Medical Expenses - expenses incurred for medical or surgical treatment. Expenses are limited to physician fees,
X-rays and emergency room services. Includes treatment for dental repair to sound natural teeth if repair is
diagnosed by a dentist as necessary and as a result of injury
Outpatient Physician’s Treatment - treatment outside the hospital for any cause. Payable up to 2 visits per
covered person, per calendar year and a maximum of 4 visits per calendar year if dependents are covered
ADDITIONAL BENEFITS
Hospital Admission** -
first hospital confinement occurring during a calendar year, and 12 months after the eective
date. Payable when a benefit has been paid under the Hospital Confinement Benefit in the base policy
Lacerations** -
treatment for one or more lacerations (cuts)
Burns** -
treatment for one or more burns, other than sunburns
Skin Graft - receiving a skin graft
for which a benefit is paid under the Burns benefit
Brain Injury Diagnosis** -
first diagnosis of concussion, cerebral laceration, cerebral contusion or intracranial
hemorrhage
within three days of an accident. Must be diagnosed within 30 days after the accident by CT Scan, MRI, EEG, PET
scan or X-ray
Computed Tomography (CT) Scan and Magnetic Resonance Imaging (MRI)* -
must first be treated by a
physician within 30 days after the accident
Paralysis** -
spinal cord injury resulting in complete/permanent loss of use of two or more limbs for at least 90 days
Coma with Respiratory Assistance -
unconsciousness lasting 7 or more days; intubation required. Medically
induced comas excluded
Open Abdominal or Thoracic Surgery
3,
**
Tendon, Ligament, Rotator Cu or Knee Cartilage Surgery
3
,
* -
surgery received for torn, ruptured, or severed
tendon, ligament, rotator cu or knee cartilage; pays the reduced amount shown for arthroscopic exploratory surgery
Ruptured Disc Surgery
3
,
* -
diagnosis and surgical repair to a ruptured disc of the spine by a physician
Eye Surgery -
surgery or removal of a foreign object by a physician
General Anesthesia* -
payable only if the policy Surgery benefit is paid
Blood and Plasma** -
transfusion after an accident
Appliance -
physician-prescribed wheelchair, crutches or walker to help with personal locomotion or mobility
Medical Supplies -
purchased over-the-counter medical supplies. Payable only if the policy Medical Expenses
benefit is paid
Medicine -
purchased prescription or over-the-counter medicines. Payable only if the policy Medical Expenses
benefit is paid
Prosthesis* -
physician-prescribed prosthetic arm, leg, hand, foot or eye lost as a result of an accident. Payable only
if a benefit is paid for loss of arm, leg, hand, foot or eye under the Dismemberment benefit
Physical Therapy* -
one treatment per day; maximum of 6 treatments per accident.
Chiropractic services are
excluded. Not payable for same visit for which Accident Follow-Up Treatment benefit is paid. Must take place no
longer than 6 months after accident
Rehabilitation Unit
4
-
must be hospital-confined due to an injury immediately prior to being transferred to rehab.
Not payable for the days on which the Hospital Confinement benefit is paid
Non-Local Transportation
2
-
treatment obtained at a non-local hospital or freestanding treatment center more than 100
miles from your home. Does not cover ambulance or physician’s oce or clinic visits for services other than treatment
Family Member Lodging -
one adult family member to be with you while you are confined in a non-local hospital or
freestanding treatment center
. Not payable if family member lives within 100 miles one-way of the treatment facility. Up to
30 days per accident. Only payable if the Non-Local Transportation benefit is paid
Post-Accident Transportation - after a three-day hospital stay more than 250 miles from your home, with a flight on
a common carrier to return home. Payable only if a benefit is paid for Hospital Confinement
Accident Follow-Up Treatment
5
-
must take place no longer than 6 months after the accident. Payable only if the
policy Medical Expenses benefit is paid. Not payable for the same visit for which the Physical Therapy benefit is paid
19

This brochure is for use in enrollments sitused in FL and is incomplete without the accompanying rate insert.
Rev. 9/18. This material is valid as long as information remains current, but in no event later than September 15, 2021.
Group Accident benefits are provided under policy form GVAP1, or state variations thereof.
The coverage provided is limited benefit supplemental accident insurance. The policy is not a Medicare Supplement Policy.
If eligible for Medicare, review Medicare Supplement Buyer’s Guide available from Allstate Benefits. There may be instances
when a law requires that benefits under this coverage be paid to a third party, rather than to you. If you or a dependent have
coverage under Medicare, Medicaid, or a state variation, please refer to your health insurance documents to confirm whether
assignments or liens may apply.
This is a brief overview of the benefits available under the group policy underwritten by American Heritage Life Insurance
Company (Home Oce, Jacksonville, FL). Details of the coverage, including exclusions and other limitations are included in
the certificates issued. For additional information, you may contact your Allstate Benefits Representative.
The coverage does not constitute comprehensive health insurance coverage (often referred to as “major medical
coverage”) and does not satisfy the requirement of minimum essential coverage under the Aordable Care Act.
Allstate Benefits is the marketing
name used by American Heritage
Life Insurance Company, a subsidiary
of The Allstate Corporation. ©2018
Allstate Insurance Company.
www.allstate.com or
allstatebenefits.com
CERTIFICATE SPECIFICATIONS
Conditions and Limits
When an injury results in a covered loss within 90 days (
unless otherwise stated on the Benefits page)
from the date of an accident and is diagnosed by a physician, Allstate Benefits will pay benefits as
stated. Treatment must be received in the United States or its territories.
Eligibility
Your employer decides who is eligible for your group (such as length of service and hours worked each week).
Dependent Eligibility/Termination
Coverage may include you, your spouse or domestic partner, and your children. Coverage for children
ends
when the child reaches age 26, unless he or she continues to meet the requirements of an eligible
dependent. Spouse/domestic partner coverage ends upon valid decree of divorce/termination of the
domestic partnership or your death.
When Coverage Ends
Coverage under the policy ends on the earliest of: the date the policy or certificate is canceled; the last
day of the period for which you made any required contributions; the last day you are in active
employment, except as provided under the Temporarily Not Working provision; the date you are no
longer in an eligible class; or the date your class is no longer eligible.
Continuation of Coverage
You may be eligible to continue coverage when coverage under the policy ends. Refer to your Certificate
of Insurance for details.
EXCLUSIONS AND LIMITATIONS
Benefits are not paid for: injury incurred before the eective date; act of war or participation in a riot,
insurrection or rebellion; suicide or attempt at suicide; injury while under the influence of alcohol or any
narcotic, unless taken upon the advice of a physician; any bacterial infection (except pyogenic infections
from an accidental cut or wound);
participation in aeronautics unless a fare-paying passenger on a licensed
common-carrier aircraft; committing
or attempting an assault or felony; driving in any race or speed test or
testing any vehicle on any racetrack or speedway; hernia, including complications; serving as an active
member of the Military, Naval, or Air Forces of any country or combination of countries.

Offered to the employees of:
Pasco County Schools
Group Voluntary Accident (GVAP1)
On- and O-the-Job Accident Insurance from Allstate Benefits
EE = Employee; EE + SP = Employee + Spouse;
EE + CH = Employee + Child(ren); F = Family
Injury Benefit Schedule is on reverse
PLAN PREMIUMS
Issue ages: 18 and over if actively at work
BENEFIT AMOUNTS
Benefits are paid once per accident unless otherwise noted here or in the brochure
ABJ30901X-1-Insert-PascoCS
MODE EE EE + SP EE + CH F
Semi-Monthly $7.26 $13.44 $12.30 $18.48
Monthly $14.52 $26.88 $24.60 $36.96
20thly $8.71 $16.13 $14.76 $22.18
BASE POLICY BENEFITS
PLAN
Accidental Death Employee $100,000
Spouse $50,000
Children $25,000
Common Carrier Accidental Death
Employee $500,000
(fare-paying passenger) Spouse $250,000
Children $125,000
Dismemberment
1
Employee $200,000
Spouse $100,000
Children $50,000
Dislocation or Fracture
1
Employee $8,000
Spouse $4,000
Children $2,000
Initial Hospitalization Confinement (pays once) $2,000
Hospital Confinement (pays daily) $800
Intensive Care (pays daily) $1,600
Ambulance Services Ground $800
Air $2,400
Medical Expenses (pays up to amount shown) $600
Outpatient Physician’s Treatment (pays per visit) $50
ADDITIONAL
BENEFITS
PLAN
Hospital Admission (pays once/year) $2,000
Lacerations
(pays once/year) $200
Burns < 15% body surface $400
15% or more $2,000
Skin Graft (% of Burns Benefit) 50%
Brain Injury Diagnosis (pays once) $600
Computed Tomography (CT) Scan and
$100
Magnetic Resonance Imaging (MRI)
(pays once/accident/year)
Paralysis (pays once) Paraplegia $15,000
Quadriplegia $30,000
Coma with Respiratory Assistance (pays once) $20,000
Open Abdominal or Thoracic Surgery $5,000
Tendon, Ligament, Rotator Cu Surgery $2,500
or Knee Cartilage Surgery Exploratory $750
Ruptured Disc Surgery $2,500
Eye Surgery $400
General Anesthesia $400
Blood and Plasma $1,200
Appliance $500
Medical Supplies $20
Medicine $20
Prosthesis 1 device $1,000
2 or more devices $2,000
Physical Therapy (pays daily) $120
Rehabilitation Unit (pays daily) $400
Non-Local Transportation $800
Family Member Lodging (pays daily) $200
Post-Accident Transportation (pays once/year) $400
Accident Follow-Up Treatment (pays daily) $200
Up to amount shown; see Injury Benefit Schedule on reverse. Multiple losses from same
injury pay only up to amount shown above.
21

INJURY BENEFIT SCHEDULE
Benefit amounts for coverage and one occurrence are shown below.
Covered spouse gets 50% of the amounts shown and children 25%.
For use in enrollments sitused in: FL. This rate insert is part of form ABJ30901X-1 and is not to be used on its own.
This material is valid as long as information remains current,
but in no event later than September 15, 2021.
Allstate Benefits is the marketing name used by American Heritage Life Insurance Company (Home Oce, Jacksonville, FL),
a subsidiary of The Allstate Corporation. ©2018 Allstate
Insurance Company. www.allstate.com or allstatebenefits.com.
COMPLETE DISLOCATION PLAN
Hip joint $8,000
Knee or ankle joint
, bone or bones of the foot
$3,200
Wrist joint $2,800
Elbow joint $2,400
Shoulder joint $1,600
Bone or bones of the hand
, collarbone $1,200
Two or more fingers or toes $560
One finger or toe $240
COMPLETE, SIMPLE OR CLOSED FRACTURE PLAN
Hip, thigh (femur), pelvis
$8,000
Skull
$7,600
Arm, between shoulder and elbow (shaft),
$4,400
shoulder blade (scapula), leg (tibia or fibula)
Ankle, knee cap (patella), forearm (radius or ulna), collarbone (clavicle) $3,200
Foot
, hand or wrist
$2,800
Lower jaw
$1,600
Two or more ribs, fingers or toes, bones of face or nose $1,200
One rib, finger or toe, coccyx $560
LOSS PLAN
Life $100,000
Both eyes, hands, arms, feet, or legs, or one hand
$200,000
or arm and one foot or leg
One eye, hand, arm, foot, or leg $100,000
One or more entire toes or fingers $20,000
Knee joint (except patella). Bone or bones of the foot (except toes). Bone or bones of the
hand (except fingers).
Pelvis (except coccyx). Skull (except bones of face or nose). Foot
(except toes). Hand or wrist (except fingers). Lower jaw (except alveolar process).

Protection for the
treatment of cancer and
29 specified diseases
Receiving a cancer diagnosis can be one of life’s most frightening events.
Unfortunately, statistics show you probably know someone who has been
in this situation.
With Cancer insurance from Allstate Benefits, you can rest a little easier. Our coverage
pays you a cash benefit to help with the costs associated with treatments, to pay for
daily living expenses, and more importantly, to empower you to seek the care you need.
Here’s How It Works
You choose the coverage that’s right for you and your family. Our Cancer insurance pays
cash benefits for cancer and 29 specified diseases to help with the cost of treatments
and expenses as they happen. Benefits are paid directly to you unless otherwise assigned.
With the cash benefits you can receive from this coverage, you may not need to use
the funds from your Health Savings Account (HSA) for cancer or specified disease
treatments and expenses.
Meeting Your Needs
• Guaranteed Issue, meaning no medical questions to answer at initial enrollment*
• Includes coverage for cancer and 29 specified diseases
• Benefits are paid directly to you unless otherwise assigned
• Coverage available for dependents
• Waiver of premium after 90 days of disability due to cancer for as long as your
disability lasts (employee only)
• Coverage may be continued; refer to your certificate for details
• Additional benefits have been added to enhance your coverage
With Allstate Benefits, you can protect your finances if faced with an unexpected
cancer or specified disease diagnosis. Are you in Good Hands? You can be.
Cancer Insurance
1
Life After Cancer: Survivorship by the Numbers, American Cancer Society, 2017.
2
Cancer Treatment & Survivorship
Facts & Figures, 2016-2017. *Enrolling after your initial enrollment period requires evidence of insurability.
Oered to the employees of:
Pasco County
Schools
ABJ30903X-1
DID YOU
KNOW
The number of cancer survivors in the
U.S. is increasing, and is expected to
jump to nearly 20.3 million by 2026
2
?
Early detection, improved treatments
and access to care are factors that
influence cancer survival
1
20.3 million
23
Here’s how Tony’s story of diagnosis and treatment turned into a happy ending,
because he had supplemental Cancer Insurance to help with expenses.
Tony undergoes his annual wellness test and is
diagnosed for the first time with prostate cancer.
His doctor reviews the results with him and
recommends pre-op testing and surgery.
Here’s Tony’s treatment path:
• Tony travels to a specialized hospital 400 miles
from where he lives and undergoes pre-op testing
• He is admitted to the hospital for laparoscopic
prostate cancer surgery
• Tony undergoes surgery and spends several hours
in the recovery waiting room
• He is transferred to his room where he is visited
by his doctor during a 2-day hospital stay
•
Tony is released under doctor required treatment
and care during a 2-month recovery period
Tony continues to fight his cancer and follow his
doctor recommended treatments.
CHOOSE CLAIMUSE
Tony chooses benefits to help
protect himself and his wife
if diagnosed with cancer or a
specified disease
Meet Tony
Tony is like anyone else who has been
diagnosed with cancer. He is concerned
about his wife and how she will cope
with his disease and its treatment. Most
importantly, he worries about how he
will pay for his treatment.
Here is what weighs heavily on his mind:
• Major medical only pays a portion of the
expenses associated with my treatment
• I have copays I am responsible for until
I meet my deductible
• If I am not working due to treatments,
I must cover my bills, rent/mortgage,
groceries and other daily expenses
• If the right treatment is not available
locally, I will have to travel to get the
treatment I need
Tony’s Cancer claim paid him cash
benefits for the following:
Cancer Screening
Cancer Initial Diagnosis
Continuous Hospital Confinement
Non-Local Transportation
Surgery
Anesthesia
Inpatient Drugs and Medicine
Physician’s Attendance
Comfort/Anti-Nausea
For a listing of benefits and benefit
amounts, see your company’s
rate insert.
24
Benefits (subject to maximums as listed on the attached rate insert)
HOSPITAL CONFINEMENT AND RELATED BENEFITS
Continuous Hospital Confinement - inpatient admission and confinement, up to 70 days per continuous
confinement
Extended Benefits - daily benefit for continuous hospital confinement lasting more than 70 days. Paid in lieu of all
other benefits except Waiver of Premium
Government or Charity Hospital - confinements in lieu of all other benefits except Waiver of Premium
Private Duty Nursing Services - full-time nursing services authorized by attending physician
Extended Care Facility - confinement must begin within 14 days of a covered hospital stay; payable up to the
number of days of the previous hospital stay
At Home Nursing -
private nursing care must begin within 14 days of a covered hospital stay; payable up to the
number of days of the previous hospital stay
Hospice Care (Freestanding Hospice Care Center or Hospice Care Team) -
terminal illness care in a
facility or at home; one visit per day. Must begin within 14 days of a covered hospital stay
RADIATION/CHEMOTHERAPY
Radiation/Chemotherapy -
covered treatments to destroy or modify cancerous tissue
Blood, Plasma and Platelets -
transfusions, administration, processing, procurement, cross-matching
SURGERY AND RELATED BENEFITS
Surgery* -
based on Certificate Schedule of Surgical Procedures. Does not pay for surgeries covered by other policy benefits
Anesthesia - 25% of Surgery benefit for anesthesia received by an anesthetist
Bone Marrow or Stem Cell Transplant
- autologous, non-autologous for treatment of cancer or specified disease
other than Leukemia, or non-autologous for treatment of Leukemia
Ambulatory Surgical Center -
payable only if Surgery benefit is paid
Second Surgical Opinion -
second opinion for surgery by a doctor not in practice with your doctor
TRANSPORTATION AND LODGING BENEFITS
Ambulance - transfer by a licensed service or hospital-owned ambulance to or from hospital where confined for
cancer or specified disease treatment
Non-Local Transportation -
obtaining treatment not available locally
Outpatient Lodging -
more than 100 miles from home
Family Member Lodging and Transportation - adult family member travels with you during non-local hospital
stays for specialized treatment. Transportation not paid if Non-Local Transportation benefit paid
MISCELLANEOUS BENEFITS
Inpatient Drugs and Medicine -
not including drugs/medicine covered under the Radiation/Chemotherapy benefit
Physician’s Attendance - one inpatient visit by one physician
Physical or Speech Therapy - to restore normal body function
New or Experimental Treatment -
payable if physician judges to be necessary and only for treatment not covered
under other policy benefits
Prosthesis - surgical implantation of prosthetic device for each amputation and breast reconstructive surgery
incident to mastectomies
Comfort/Anti-Nausea Benefit -
prescribed anti-nausea medication administered on outpatient basis
Waiver of Premium** - must be disabled 90 days in a row due to cancer, as long as disability lasts
ADDITIONAL BENEFITS
Cancer Initial Diagnosis - for first-time diagnosis of cancer other than skin cancer
Intensive Care (ICU) a. ICU Confinement - confinements up to 45 days/stay
b. Ambulance - licensed air or surface ambulance service to ICU
Cancer Screening - pays annually for each covered person, when one of the following covered screening tests is
performed: Bone Marrow Testing; Blood Tests for CA15-3 (breast cancer), CA125 (ovarian cancer), PSA (prostate
cancer) and CEA (colon cancer); Chest X-ray; Colonoscopy; Flexible Sigmoidoscopy; Hemoccult Stool Analysis;
Mammography; Pap Smear; Serum Protein Electrophoresis (test for myeloma)
SPECIFIED DISEASES
29 Specified Diseases Covered -
Amyotrophic Lateral Sclerosis (Lou Gehrig’s Disease), Muscular Dystrophy,
Poliomyelitis, Multiple Sclerosis, Encephalitis, Rabies, Tetanus, Tuberculosis, Osteomyelitis, Diphtheria, Scarlet Fever,
Cerebrospinal Meningitis, Brucellosis, Sickle Cell Anemia, Thalassemia, Rocky Mountain Spotted Fever, Legionnaires’
Disease, Addison’s Disease, Hansen’s Disease, Tularemia, Hepatitis (Chronic B or C), Typhoid Fever, Myasthenia
Gravis, Reye’s Syndrome,
Primary Sclerosing Cholangitis (Walter Payton’s Disease), Lyme Disease, Systemic Lupus
Erythematosus, Cystic Fibrosis, and Primary Biliary Cirrhosis
*Two or more surgeries done at the same time are considered one operation. The operation with the largest benefit
will be paid. Outpatient is paid at 150% of the amount listed in the Schedule of Surgical Procedures. Does not pay
for other surgeries covered by other benefits **Premiums
waived for employee only
Using your cash benefits
Cash benefits provide you with
options, because you decide
how to use them.
Finances
Can help protect HSAs,
savings, retirement
plans and 401(k)s
from being depleted.
Trave l
Can help pay for expenses
while
receiving treatment
in another city.
Home
Can help pay the
mortgage, continue
rental payments, or
perform needed
home
repairs for after care.
Expenses
Can help pay your family’s
living expenses such as
bills, electricity, and gas.
An easy-to-use website that
offers 24/7 access to important
information
about your benefits.
Plus, you can submit
and check
your claims (including claim
history), request your cash
benefit to be direct deposited,
make changes to personal
information, and more.
Eligibility
Coverage may include you, your
spouse, and children.
MyBenefits: 24/7 Access
allstatebenefits.com/mybenefits
25

This brochure is for use in enrollments sitused in FL and is incomplete without the accompanying rate insert.
Rev. 9/18. This material is valid as long as information remains current, but in no event later than September 15, 2021.
Group Cancer benefits are provided under policy form GVCP2, or state variations thereof.
The coverage provided is limited benefit supplemental cancer and specified disease insurance. The policy is not a
Medicare Supplement Policy. If eligible for Medicare, review Medicare Supplement Buyer’s Guide available from
Allstate Benefits. There may be instances when a law requires that benefits under this coverage be paid to a third
party, rather than to you. If you or a dependent have coverage under Medicare, Medicaid, or a state variation, please
refer to your health insurance documents to confirm whether assignments or liens may apply.
This is a brief overview of the benefits available under the group policy underwritten by American Heritage Life
Insurance Company (Home Oce, Jacksonville, FL). Details of the coverage, including exclusions and other limitations
are included in the certificates issued. For additional information, you may contact your Allstate Benefits Representative.
The coverage does not constitute comprehensive health insurance coverage (often referred to as “major medical
coverage”) and does not satisfy the requirement of minimum essential coverage under the Aordable Care Act.
Allstate Benefits is the marketing
name used by American Heritage
Life Insurance Company, a subsidiary
of The Allstate Corporation. ©2018
Allstate Insurance Company.
www.allstate.com or
allstatebenefits.com
CERTIFICATE SPECIFICATIONS
Eligibility
Coverage may include you, your spouse, and children.
Termination of Coverage
Coverage under the policy ends on the date the policy is canceled; the last day premium payments were
made; the last day of active employment; or the date you or your class is no longer eligible.
Spouse coverage ends upon divorce or your death. Coverage for children ends when the child reaches
age 26, unless he or she continues to meet the requirements of an eligible dependent.
Conversion Privilege
If coverage terminates for any reason other than non-payment of premiums, the covered person can convert
to an individual policy without evidence of insurability. This may also apply to a dependent whose coverage
terminates.
LIMITATIONS AND EXCLUSIONS
Pre-Existing Condition Limitation
We do not pay benefits for a pre-existing condition during the 12-month period beginning on the date that
person’s coverage starts.
A pre-existing condition is a disease or physical condition for which medical
advice or treatment was received by the covered person during the 6-month period prior to the eective
date of coverage.
Exclusions and Limitations
We do not pay for any loss except for losses due directly from cancer or a specified disease and any
other conditions or diseases caused or aggravated by cancer or a specified disease. Treatment and
services must be received in the United States or its territories.
For those benefits for which we pay actual charges up to a specified maximum amount (except
Radiation/Chemotherapy; Blood, Plasma and Platelets; Prosthesis; New or Experimental Treatment;
and Bone Marrow or Stem Cell Transplant), if specific charges are not obtainable as proof of loss, we
will pay 50% of the maximum benefit.
Hospice Care: Services are not covered for food or meals, well-baby care, volunteers or support for the
family after covered person’s death.
Blood, Plasma and Platelets Limitation:
Does not include blood replaced by donors.
For the Radiation/Chemotherapy benefit, we do not pay for: treatment planning, consultation or
management; the design and construction of treatment devices; basic radiation dosimetry calculation;
any type of laboratory tests; X-ray or other imaging used for diagnosis or monitoring; the diagnostic tests
related to these treatments; or any devices or supplies including intravenous solutions and needles
related to these treatments.
We do not pay the Family Member Transportation Benefit if we pay the personal vehicle transportation
benefit under the Non-Local Transportation Benefit when the family member lives in the same town as
the confined insured.
Intensive Care Exclusions and Limitations
Benefits are not paid for attempted suicide or intentional self-inflicted injury, intoxication or being under
the influence of drugs not prescribed by a physician, or alcoholism or drug addiction. Benefits are not paid
for confinements to a care unit that does not qualify as a hospital intensive care unit, including progressive
care, subacute intensive care, intermediate care, private rooms with monitoring, or step-down and other
lesser care units. Benefits are not paid for continuous confinements occurring during a hospitalization prior
to the eective date. We do not pay for ambulance if paid under the Ambulance benefit (see Transportation
and Lodging benefit section of this brochure).
DEFINITIONS
Actual Charges vs. Actual Cost
Actual Charge –
Amount billed
for a treatment or service before
any insurance discounts or
payments.
Actual Cost – Amount actually
paid by or on behalf of you,
accepted as full payment by
the
provider of goods or services.

For use in enrollments sitused in: FL
This rate insert is part of form ABJ30903X-1 and is not to be used on its own.
This material is valid as long as information remains current,
but in no event later than September 15, 2021. Allstate Benefits is
the marketing name used by American Heritage Life Insurance Company (Home Office, Jacksonville, FL), a subsidiary of
The Allstate Corporation. ©2018 Allstate Insurance Company. www.allstate.com or allstatebenefits.com.
ABJ30903X-1-Insert-PascoCS
Offered to the employees of:
Pasco County Schools
MODE EE F
Semi-Monthly $7.44 $12.70
Monthly $14.87 $25.40
20thly $8.92 $15.24
PLAN 1 PREMIUMS
EE = Employee; F = Family
Issue Ages: 18 and over if Actively at Work
Cancer Insurance (GVCP2)
Includes coverage for 29 Specified Diseases
from Allstate Benefits
BENEFIT AMOUNTS
1
Pays actual charges up to amount listed.
2
Pays actual charges up to amount listed in certificate
Schedule of Surgical Procedures. Amount paid depends on surgery.
3
Pays actual cost up to amount
listed.
Maximum of 700 miles.
HOSPITAL CONFINEMENT AND RELATED BENEFITS
PLAN 1
PLAN 2
Continuous Hospital Confinement (daily) $200 $300
Extended Benefits
1
(daily) $200 $300
Government or Charity Hospital (daily) $200 $300
Private Duty Nursing Services
1
(daily) $200 $300
Extended Care Facility
1
(daily) $200 $300
At Home Nursing
1
(daily) $200 $300
Hospice Care Center
1
(daily) or $200 $300
Hospice Care Team
1
(per visit) $200
$300
RADIATION/CHEMOTHERAPY
PLAN 1
PLAN 2
Radiation/Chemotherapy
1
(every 12 months)
$5,000 $10,000
Blood, Plasma, and Platelets
1
(every 12 months)
$5,000 $10,000
SURGERY AND RELATED BENEFITS
PLAN 1
PLAN 2
Surgery
2
1. Inpatient $1,500 $4,500
2. Outpatient $2,250 $6,750
Anesthesia
1
(% of surgery benefit) 25%
25%
Bone Marrow or Stem Cell Transplant (once/year)
1. Autologous 1. $500 1. $1,500
2. Non-autologous (cancer or specified disease treatment) 2. $1,250 2. $3,750
3. Non-autologous (Leukemia) 3. $2,500 3. $7,500
Ambulatory Surgical Center
1
(daily) $250 $750
Second Surgical Opinion
1
$200 $600
TRANSPORTATION AND LODGING BENEFITS
PLAN 1
PLAN 2
Ambulance
1
(per confinement) $100 $100
Non-Local Transportation
(coach fare or amount shown per mile
)
$0.40/mi
$0.40/mi
Outpatient Lodging
3
(daily; limit $2,000/12 mo. period)
$50 $50
Family Member Lodging
3
(daily per trip; max. 60 days) $50 $50
and Transportation
(coach fare or amount shown per mile
)
$0.40/mi
$0.40/mi
MISCELLANEOUS BENEFITS
PLAN 1
PLAN 2
Inpatient Drugs and Medicine
1
(daily)
$25
$25
Physician’s Attendance
1
(daily)
$50
$50
Physical or Speech Therapy
1
(daily)
$50
$50
New or Experimental Treatment
1
(every 12 months)
$5
,000
$5
,000
Prosthesis
1
(per amputation)
$2
,000
$2
,000
Comfort/Anti-Nausea Benefit
1
$200 $200
Waiver of Premium (employee only) Ye s Yes
ADDITIONAL BENEFITS
PLAN 1
PLAN 2
Cancer Initial Diagnosis (one-time benefit) $2,000 $5,000
Intensive Care (ICU)
ICU Confinement
(daily)
$200 $600
Ambulance Charges Charges
Cancer Screening
$50
$100
MODE EE F
Semi-Monthly $15.83 $27.28
Monthly $31.65 $54.56
20thly $18.99 $32.74
PLAN 2 PREMIUMS
27


29

31


DID YOU
KNOW
?
$7,500
cost to fix a broken leg
Medical costs in the United States
are among the highest in the world.
In 2015, the average cost to fix
a broken leg in the United States
was $7,500.
2
In recent years, the
cost of a hospital stay
has increased by more
than 37%.
1
$30,000
cost per 3-day stay
The average cost of a 3-day
hospital stay is around $30,000
.
3
Oered to the employees of:
Pasco County Schools
Life is unpredictable. Without any warning, an illness or injury can lead to a
hospital confinement, medical procedures and/or visits, which may mean
costly out-of-pocket expenses.
Expenses associated with a hospital stay can be financially dicult if money is tight and
you are not prepared. But having the right coverage in place before you experience
a sickness or injury can help eliminate your financial concerns and provide support at a
time when it is needed most.
Allstate Benefits oers a solution to help you protect your income and empower you to
seek treatment.
Here’s How It Works
Our Hospital Indemnity insurance pays a cash benefit for hospital confinements. This
benefit is payable directly to you and can keep you from withdrawing money from your
personal bank account or your Health Savings Account (HSA) for hospital-related expenses.
It is increasingly important to not only protect your finances if faced with an unexpected
illness, but also to empower yourself to seek the necessary treatment.
Meeting Your Needs
•
Guaranteed Issue coverage, meaning no medical questions to answer
•
Coverage also available for your dependents
•
Premiums are aordable and are conveniently payroll deducted
•
Coverage may be continued; refer to your certificate for more details
With Allstate Benefits, you can feel assured that you have the protection you need if faced
with a hospitalization.
Are you in Good Hands? You can be.
Protection for hospital
stays when a sickness
or injury occurs
ABJ30904X-1
1
http://www.uofmhealth.org/news/archive/201606/heading-hospital-even-insurance-it-may-cost-you-1000-or-more
2
www.healthcare.gov/why-coverage-is-important/protection-from-high-medical-costs/
3
www.cdc.gov/nchs/data/hus/2012/099.pdf
Hospital Indemnity Insurance
33

Tommy’s story of sickness and a hospital stay turned into a happy ending, because
his parents had supplemental Hospital Indemnity Insurance to help with expenses.
Tommy was sick and vomiting, had a loss of appetite
and a fever, and complained about a pain in his side.
He w
as also unable to get out of bed.
Here’s Tommy’s treatment path:
•
Taken by ambulance to the emergency room
• Examined by a physician
• Multiple tests were performed
• Admitted for a two-day hospital stay
• Undergoes emergency appendectomy surgery
• Visited by his doctor and
released
• Recovered from surgery in 5 weeks
•
Seen by the
doctor during a follow-up visit
Tommy’s mother went online after Tommy’s hospital
stay
to file a claim. The cash benefits were direct
deposited
into her bank account.
Tommy is fully recovered and back to normal.
CHOOSE CLAIMUSE
Tommy’s mother chooses benefits
to help
protect herself and her
family members, should they
suffer an illness or injury that
requires a hospital stay.
Meet Tommy
Tommy’s parents are like most parents;
they worry about the health and well-being
of their family. They know that as Tommy
grows he will
become more active and may
be hospitalized due to a
sickness or injury.
Most importantly, they worry about how
they will pay for it.
Here is what weighs heavily on their minds:
• Major medical only pays a portion of the
expenses associated with hospital stays
• They have copays they are responsible for
until they meet their deductible
• If they miss work due to Tommy having
a hospital stay,
they must cover their
bills, rent/mortgage,
groceries and
education expenses
• If the right treatment is not available
locally, they will have to travel to
get the treatment he needs
Tommy’s hospital stay claim paid cash
benefits for the following:
Ambulance
First Day Hospital Confinement
Daily Hospital Confinement
Variable Surgical Schedule
Anesthesia
Inpatient Physician’s Treatment
Outpatient Physician’s Treatment
For a listing of benefits and benefit
amounts, see the rate insert.
Benefits
HOSPITALIZATION BENEFITS
First Day Hospital Confinement - once per continuous confinement per covered person, up to the limit stated in
the rate insert. Not paid for newborn child’s initial confinement after birth (see Hospitalization Due to Pregnancy at
bottom left for complete details)
Daily Hospital Confinement -
up to the maximum number of days for each confinement.* Hospitalization due to
pregnancy is covered, subject to any Pregnancy Waiting Period (see rate insert). Not paid for any day the First Day
Hospital Confinement benefit is paid
Hospital Intensive Care -
up to the maximum number of days for each confinement.* Pays in addition to the First
Day Hospital Confinement benefit and Daily Hospital Confinement benefit
Inpatient Physician’s Treatment - for physician services (other than a surgeon) when hospital confined, up to
the maximum number of days for each confinement.* Payable once per day per covered person
SURGERY BENEFITS
Variable Surgical Schedule - surgery performed in a hospital or ambulatory surgical center, based on the
amount shown in the certificate Surgical Schedule.**
†
Payable once per day per covered person
Ambulatory Surgical Center -
surgery performed at an ambulatory surgical center. Not paid for any day the
Outpatient Emergency Treatment benefit is paid. Payable once per day per covered person, up to 2 days per person
per year
Anesthesia -
25% of the Variable Surgical Schedule benefit
OUTPATIENT BENEFITS
Outpatient Emergency Treatment -
medical treatment received in an emergency treatment center. Not paid for
any day the Ambulatory Surgical Center benefit is paid. Payable once per day per covered person, up to 2 days per
person per coverage year
Outpatient Physician’s Treatment -
physician treatment received outside a hospital for any cause. Payable once
per day per covered person, up to 5 days per covered person, per coverage year; max. 10 days per coverage year if
Employee + Spouse or Employee + Child(ren); or a max. of 15 days per coverage year if Family coverage
Ambulance -
transportation by ground or air to an emergency treatment center by a licensed or hospital-owned
ambulance. Payable once per day per covered person, up to 3 days per person per coverage year
Non-Local Transportation - first day of
confinement for treatment in a non-local hospital 100 miles or more
away from home.
Payable once for each confinement, up to the limit stated in the rate insert
DIAGNOSTIC & WELLNESS BENEFITS
Fixed Outpatient Diagnostic X-ray and Laboratory -
tests performed on an outpatient basis to diagnose an
injury or sickness. Payable once per day per covered person, up to 3 days per person per year. Not paid for any day
the Fixed Wellness benefit is paid
Fixed Wellness -
once per day per person per year, if one of the following services is received: Biopsy for skin cancer;
Blood test for triglycerides;
Bone Marrow Testing; CA15-3, CA125, CEA and PSA (blood tests for breast, ovarian, colon
and prostate cancer); Chest X-ray; Colonoscopy; Doppler screenings for carotids and peripheral vascular disease;
Echocardiogram;
EKG (Electrocardiogram); Flexible sigmoidoscopy;
Hemoccult
stool analysis; HPV Vaccination
(Human Papillomavirus);
Lipid panel (total cholesterol count); Mammography, including Breast Ultrasound; Pap
Smear, including ThinPrep Pap
Test; Serum Protein Electrophoresis (test for myeloma); Stress test on bike or
treadmill; Thermography; Ultrasound screening for abdominal aortic aneurysms. Not paid for any day the Fixed
Outpatient Diagnostic X-ray and Laboratory benefit is paid
*
See the maximum number of days for each confinement on
the rate insert
. **See the full schedule located under the
Benefit Information section in your certificate; ask your benefits representative for details.
†
Two or more surgeries
performed at the same time through one incision are considered one surgery.
Using your cash benefits
Cash benefits provide you with
options, because you decide
how to use them.
Finances
Can help protect HSAs,
savings, retirement
plans and 401(k)s
from being depleted.
Trave l
Can help pay for expenses
while
receiving treatment
in another city.
Home
Can help pay the
mortgage, continue
rental payments, or
perform needed
home
repairs for after care.
Expenses
Can help pay your family’s
living expenses such as
bills, electricity, and gas.
An easy-to-use website that oers
24/7 access to important information
about your benefits. Plus, you can
submit
and check your claims
(including claim history), request
your cash benefit to be direct
deposited, make changes to personal
information, and more.
MyBenefits: 24/7 Access
allstatebenefits.com/mybenefits
Hospitalization Due to
Pregnancy
Your First Day Hospital Confinement
does include hospitalization due to
normal pregnancy or complications
of pregnancy. A newborn child’s
initial confinement in a hospital
is not payable. A newborn child’s
initial confinement in a hospital
includes any transfers to another
hospital before being discharged
to go home.
A newborn child’s routine nursing
or well-baby care during the
initial confinement in a hospital
is not payable.
Dependent Eligibility
Coverage may include you, your
spouse or domestic partner,
and children.
35

CERTIFICATE SPECIFICATIONS
Conditions and Limits
We pay benefits as stated for service and treatment received by the covered person while coverage is in
force for sickness or injury. Hospital room and board charges must be incurred for benefits to be payable.
Treatment must be received in the United States or its territories
.
Eligibility
Your employer decides who is eligible for your group (such as length of service and hours worked each
week). Issue ages are 18 and over.
Dependent Eligibility/Termination of Coverage
Coverage may include you, your spouse or domestic partner, and children. Coverage for children
ends
upon your death or when the child reaches age 26, unless he or she continues to meet the requirements
of an
eligible dependent. Spouse coverage ends upon valid decree of divorce or your death. Domestic
partner coverage
ends upon termination of domestic partnership or your death.
When Coverage Ends
Coverage under the policy ends on the earliest of: the date the policy is canceled; the last day of
the period
for which you made any required contributions; the last day you are in active employment or
a member in
an association, labor union or other entity, except as provided under the “Temporary Layo, Leave of Absence,
or Family and Medical Leave of Absence” provision; the date you are no longer in an eligible class; the
date your class is no longer eligible; or upon discovery of fraud or material misrepresentation when filing
for a claim.
Portability
You may be eligible to continue your coverage when coverage under the policy ends. Portability
coverage ends when the group policy terminates. Refer to your Certificate of Insurance for details.
Pre-Existing Condition
We do not pay benefits due to a pre-existing condition if the loss occurs during the first 12 months of
coverage. A pre-existing condition is a condition for which: medical treatment, consultation, care or services
were received, including diagnostic measures; drugs or medicines were taken or prescribed; over-the-
counter medications were taken; treatment recommendations were followed in the 12 months prior to the
eective date or the date an increase in benefits would be eective; or symptoms existed within the 12 months
prior to the eective date or the date an increase in benefits would be eective.
EXCLUSIONS AND LIMITATIONS
Benefits are not paid for: injury or sickness incurred before the eective date; any act of war or participation
in a riot, insurrection or rebellion; suicide or attempt at suicide; engaging in an illegal occupation or
committing or attempting an assault or felony; cosmetic dentistry or plastic surgery, except to treat an injury
or correct a disorder of normal body function; intentionally self-inflicted injuries; confinement that begins
before the eective date of coverage; the reversal of a tubal ligation or vasectomy; artificial insemination, in
vitro fertilization, and test tube fertilization, including any related testing, medications or physician services,
unless required by law; participation in aeronautics (including parachuting and hang gliding) unless a
fare-paying passenger on a licensed common-carrier aircraft operating between established airports; a
newborn child’s routine nursing or well-baby care during the initial confinement in the hospital; driving in
any race or speed test or testing any motorized vehicle on any racetrack or speedway; mental or nervous
disorders; alcoholism, drug addiction or dependence upon any controlled substance.
Allstate Benefits is the marketing
name used by American Heritage
Life Insurance Company, a subsidiary
of The Allstate Corporation. ©2018
Allstate Insurance Company.
www.allstate.com or
allstatebenefits.com
This brochure is for use in enrollments sitused in FL and is incomplete without the accompanying rate insert.
Rev. 9/18. This material is valid as long as information remains current, but in no event later than September 15, 2021.
Group Hospital Indemnity benefits are provided under policy form GVSP2, or state variations thereof.
The coverage provided is limited benefit hospital indemnity medical insurance. The policy is not a Medicare Supplement
Policy. If eligible for Medicare, review Medicare Supplement Buyer’s Guide available from Allstate Benefits. There may be
instances when a law requires that benefits under this coverage be paid to a third party, rather than to you. If you or a
dependent have coverage under Medicare, Medicaid, or a state variation, please refer to your health insurance documents
to confirm whether assignments or liens may apply.
This is a brief overview of the benefits available under the group policy underwritten by American Heritage Life Insurance
Company (Home Oce, Jacksonville, FL). Details of the coverage, including exclusions and other limitations are included
in the certificates issued. For additional information, you may contact your Allstate Benefits Representative.
The coverage does not constitute comprehensive health insurance coverage (often referred to as “major medical
coverage”) and does not satisfy the requirement of minimum essential coverage under the Aordable Care Act.

Offered to the employees of:
Pasco County Schools
Hospital Indemnity (GIM2)
Group Hospital Indemnity Insurance
from Allstate Benefits
BENEFIT AMOUNTS
For use in the Pasco County Schools enrollment sitused in: FL
This rate insert is part of form ABJ30904X-1 and is not to be used on its own.
This material is valid as long as information remains current,
but in no event later than September 15, 2021. Allstate Benefits is
the marketing name used by American Heritage Life Insurance Company (Home Office, Jacksonville, FL), a subsidiary of
The Allstate Corporation. ©2018 Allstate Insurance Company. www.allstate.com or allstatebenefits.com.
ABJ30904X-1-Insert-PascoCS
EE = Employee; EE + SP = Employee + Spouse;
EE + CH = Employee + Child(ren); F = Family
Issue Ages: 18 and over if Actively at Work
PLAN 1 PREMIUMS
PLAN 2 PREMIUMS
MODE EE EE + SP EE + CH F
Semi-Monthly $19.37 $42.06 $33.48 $47.78
Monthly $38.74 $84.11 $66.95 $95.55
20thly $23.24 $50.47 $40.17 $57.33
MODE EE EE + SP EE + CH F
Semi-Monthly $40.30 $88.66 $69.75 $100.36
Monthly $80.60 $177.32 $139.49 $200.72
20thly $48.36 $106.39 $83.69 $120.43
HOSPITALIZATION BENEFITS PLAN 1
PLAN 2
First Day Hospital Confinement
$650 $1,450
Limit to Number of Occurrences
Once/30 days Once/30 days
Daily Hospital Confinement (daily)
$200 $450
Maximum Number of Days 30 30
Hospital Intensive Care (daily)
$200 $450
Maximum Number of Days 30 30
Inpatient Physician’s Treatment (daily) n/a $75
Maximum Number of Days n/a 30
SURGERY BENEFITS PLAN 1
PLAN 2
Variable Surgical Schedule (daily, varies by surgery) n/a
$100-$4,000
Ambulatory Surgical Center (daily) $50 $50
Anesthesia (% of Surgical Schedule) n/a 25%
OUTPATIENT BENEFITS PLAN 1
PLAN 2
Outpatient Emergency Treatment (daily) $50 $100
Outpatient Physician’s Treatment (daily) $50 $75
Ambulance (daily)
Ground
n/a
$100-$200
Air
n/a
$200-$400
Non-Local Transportation
n/a
$50
Limit to Number of Occurrences
n/a
No Limit
DIAGNOSTIC & WELLNESS BENEFITS PLAN 1
PLAN 2
Fixed Outpatient Diagnostic X-ray and Laboratory (daily)
$50
$100
Fixed Wellness (daily)
$50
$100
37

A death not only leaves behind loved ones, but can also leave overwhelming financial
obligations. And, if you’re like most people, you don’t have enough life insurance to
keep your family afloat if an unexpected death occurs. Give yourself and your loved
ones a gift of love – put yourself in Good Hands with coverage from Allstate Benefits.
Without a Term Life Insurance policy, your family may have to tap into their savings,
retirement, or 401k to help cover final expenses and everyday living expenses, should
a
breadwinner die unexpectedly. This product oers a guaranteed premium to age 100.
Here’s How It Works
You choose the coverage that’s right for you and your family. With planning, the death
benefit can pass to your beneficiaries free from state or federal estate taxes. Consult
with your tax advisor for specific information. Then, when life comes to an end, your
beneficiary can receive a tax-free death benefit that can be used to help pay for funeral
expenses, mortgage payments and more.
Meeting Your Needs
• You choose the death benefit amount to leave behind
• Coverage for spouse through a separate certificate, and for child(ren) through a
separate certificate or rider
• Premiums are aordable and remain level to age 100 unless you make changes to
your coverage
• Premiums are aordable and conveniently payroll deducted
• Guaranteed minimum death benefit is level for 5 years; current non-guaranteed
death benefit is projected to remain level to age 100
With Allstate Benefits, you gain peace of mind knowing your loved ones will receive a
financial safety net when you die – think of it as your final gift of love.
Are you in Good Hands? You can be.
Term to Age 100 Life Insurance
DID YOU
KNOW
?
ABJ30905X-1
Sixty-nine percent of people
surveyed would have trouble
paying living expenses in two
years or less if they were to lose
their primary wage earner.
1
69%
A number of financial concerns
remain consistent from person to
person, including long-term care,
financial security of dependents,
credit card debt, and having a
comfortable retirement.
1
1
2017 Insurance Barometer Study, LIMRA
Protecting those you
love during life’s most
challenging
times
Oered to the employees of:
Pasco County
Schools

Tiany’s Term Life coverage brought comfort to her family, because they
received a lump-sum cash benefit to help with their everyday living expenses.
Tiany was out of town on business when she
suered a heart attack. She was rushed to the
hospital, but all of the life-saving actions by the
medical team could not save her
.
Here’s Tiany’s treatment path:
• Tiany traveled out of town on business
• She was meeting with a client when sharp pains
and shortness of breath caused her to collapse
• She was taken by ambulance to the nearest
hospital emergency room
• While in the emergency room, her heart began
beating at an altered rate, then stopped
•
The emergency room doctors and nurses worked
tirelessly to revive her, but they could not save her
•
Her husband and family were notified of her passing
Tiffany’s family used proceeds from the lump-sum
cash benefit to cover her final expenses.
CHOOSE CLAIMUSE
Tiffany chooses a Term Life
policy to help protect her
family in the event of her
untimely death.
Meet Tiany
Tiany is like any parent who has
emotional and financial responsibilities.
She’s worried about how her family
will make ends meet if she dies
unexpectedly. Most importantly,
she worries about leaving them
with a large debt.
Here is what weighs heavily on her mind:
• She has a mortgage and still owes a
substantial amount before it is paid o
• Her children go to private school and
will need income to help continue their
education as they get older
• Her debt to income ratio is high and
would be a hardship on her family
• Daily living expenses for items such
as gas, food, insurance, electricity,
and water are a necessary part of life
•
Funeral expenses are high and the
government provides very little
for assistance
Tiany designated her husband as her
beneficiary. He received the following:
Term Life: Lump-sum cash benefit
The cash benefit was direct deposited
into his bank account.
For complete details on the benefits
and pricing, please consult with your
benefits representative
.
39
Using your cash benefits
Cash benefits provide you with
options, because you or your
beneficiary get to decide
how to use them.
Finances
Can help eliminate the
need to
deplete savings or
retirement plans
Home
Can help pay the
mortgage, continue
rental payments, or
perform needed
home
repairs
Expenses
Can help pay your family’s
living expenses such as
bills, electricity and gas
An easy-to-use website that
offers 24/7 access to important
information
about your benefits.
Plus, you can submit
and check
your claims (including claim
history), request your cash
benefit to be direct deposited,
make changes to personal
information, and more.
MyBenefits: 24/7 Access
AllstateBenefits.com/mybenefits
Benefits Issue Ages
EE/SP
2
Term Life Insurance Death Benefit -
pays a lump-sum death benefit to 18-80 NT & 19-80 T
your designated beneficiary when you die before age 100 CH/GCH
2
0-25 NT & 19-25 T
EE = Employee, SP = Spouse, CH = Children, GCH = Grandchildren, NT = Non-Tobacco, T = Tobacco
2
Coverage for spouse and child(ren) may be limited to a percentage of the employee’s face amount.
ADDITIONAL RIDER BENEFIT
3
Insured Issue Ages
Accelerated Death Benefit for Terminal Illness - an advance of the
0-75
death benefit is paid when diagnosed as terminally ill
3
The rider listed has exclusions and limitations.
Why Term Life Insurance might be right for you
Have you ever experienced a life-changing event, whether good or bad, and worried that you would
not have the finances in place to handle it if you lost your spouse?
Perhaps it has crossed your mind, but you put it o because you did not want to think about the
unthinkable. However, if you have a spouse, children, or even grandchildren, that is reason enough to
think about planning for their future today.
Here are some additional reasons to consider:
• You can’t predict when you’ll die, whether from a disease, accidental injury or natural causes
Upon your death, Term to Age 100 can provide a lump-sum cash benefit directly to your designated beneficiary
• You live on a budget, and purchasing traditional permanent life insurance would be costly
Term to Age 100 is affordably priced
• You want
a Term Life policy that oers coverage for more than 5, 10 or 20 years
Term to Age 100 offers coverage that can be with you until age 100
• You want aordable coverage that goes with you should you leave your employer
You can take the Term to Age 100 coverage with you; see your Certificate of Insurance for details
• You’re the primary wage earner and your family would have diculty living without your income
If you die before age 100, Term to Age 100 offers your designated beneficiary a lump-sum death benefit that
is
guaranteed for the first five years of coverage and is priced to remain level under current experience factors
• You have recurring monthly debts such as a mortgage, car payment or credit cards
Term to Age 100 provides a lump-sum death benefit that can be used to help cover monthly expenses
• You have children under 18, and they require money for daily living expenses such as food, clothing,
school sports and college education
Term to Age 100 provides a lump-sum death benefit that can be used to help with daily living expenses
• Your family may need additional money to help with health care related bills after you die
Term to Age 100 provides a lump-sum death benefit that can be used to help cover these expenses
40

EXCLUSIONS AND LIMITATIONS
Suicide Exclusion - If a covered person commits suicide, the death benefit may be limited to the
premiums paid for that covered person.
Other Exclusions and Limitations - The policy and rider have other elimination periods, exclusions and
limitations that may aect coverage. Please refer to your certificate for details.
Allstate Benefits is the marketing
name used by American Heritage
Life Insurance Company, a subsidiary
of The Allstate Corporation. ©2018
Allstate Insurance Company.
www.Allstate.com or
AllstateBenefits.com
This brochure is for use in enrollments sitused in FL.
Rev. 9/18. This material is valid as long as information remains current, but in no event later than September 15, 2021.
Group Term Life Insurance benefits are provided under policy form GPTLP, or state variations thereof. Accelerated Death
Benefit for Terminal Illness benefits are provided under rider form GTLPLBR, or state variations thereof.
This is a brief overview of the benefits available under the group policy underwritten by American Heritage Life Insurance
Company (Home Oce, Jacksonville, FL). Details of the coverage, including exclusions and other limitations are
included in the certificates issued. For additional information, you may contact your Allstate Benefits Representative.

What does it cost?
Which plan is right for you?
Legal Insurance from ARAG
UltimateAdvisor Plus™ oers you
all of the above and more including:
Wt l
e?
Legal coverage isn’t just
for the serious issues,
it’s for your everyday needs,
too. Legal insurance helps
you address common
situations like creating wills,
transferring property or
buying a home.
Me s pe!
See the complete list of what your plan covers at:
Access Code:
What does legal insurance cover?
A legal insurance plan from ARAG® covers a wide range of legal needs
like the examples shown below – and many more – to help you address
life's legal situations.
&RQVXPHU 3URWHFWLRQ
$XWR UHSDLU
%X\RUVHOODFDU
&RQVXPHU IUDXG
&RQVXPHU SURWHFWLRQ IRU
JRRGVRUVHUYLFHV
+RPH LPSURYHPHQW
3HUVRQDO SURSHUW\ GLVSXWHV
6PDOO FODLPV FRXUW
&ULPLQDO 0DWWHUV
-XYHQLOH
3DUHQWDO UHVSRQVLELOLW\
'HEW5HODWHG 0DWWHUV
'HEW FROOHFWLRQ
*DUQLVKPHQWV
3HUVRQDO EDQNUXSWF\
6WXGHQW ORDQ GHEW
'ULYLQJ 0DWWHUV
/LFHQVH VXVSHQVLRQUHYRFDWLRQ
7UDIILF WLFNHWV
7D[ ,VVXHV
,56 WD[ DXGLW
,56 WD[ FROOHFWLRQ
)DPLO\
$GRSWLRQ
*XDUGLDQVKLSFRQVHUYDWRUVKLS
1DPH FKDQJH
3HWUHODWHG PDWWHUV
'LYRUFH
6HUYLFHV IRU 7HQDQWV
&RQWUDFWVOHDVH DJUHHPHQWV
(YLFWLRQ
6HFXULW\ GHSRVLW
'LVSXWHV ZLWK D ODQGORUG
5HDO (VWDWH +RPH 2ZQHUVKLS
%X\LQJ D KRPH
'HHGV
)RUHFORVXUH
&RQWUDFWRU LVVXHV
1HLJKERU GLVSXWHV
3URPLVVRU\ QRWHV
5HDO HVWDWH GLVSXWHV
6HOOLQJ D KRPH
:LOOV (VWDWH 3ODQQLQJ
3RZHUV RI DWWRUQH\
:LOOV
SFV
/HWV 7DON &DOO $5$* DW
$5$*OHJDOFRPP\LQIR
8OWLPDWH$GYLVRUp
PRQWKO\
8OWLPDWH$GYLVRU 3OXV
70
PRQWKO\
&KLOG FXVWRG\ VXSSRUW YLVLWDWLRQ
7UXVWV
6HUYLFHV IRU SDUHQWVJUDQGSDUHQWV
$QG PRUH
b
How does legal insurance work?
when you have a legal matter.
Customer Care will walk you through your options and help you
get connected to network attorneys.
Meet with your network attorney over the phone or in person to
begin resolving your legal issue.
1
2
3
w n l
?
Most of us aren’t prepared for
the unexpected — like the
circumstances caused by the
coronavirus outbreak.
Legal insurance provides a benet
you can use to plan for it all — the
expected and unexpected times
in your life. Go online to view a
complete list of coverages and see
how a legal plan can protect you.
Why should you get legal insurance?
Use DIY Docs® to create a variety of legally valid
documents, including state-specic templates.
Work with a network attorney and attorney fees are
100% paid-in-full for most covered matters.
Address your covered legal situations with a network
attorney who is only a phone call away for legal help
and representation.
Save thousands of dollars on average, for each
legal matter by avoiding costly legal fees.*
Avoid the hassle of nding a local attorney on your
own – access more than , attorneys in ARAG’s
network who average + years of experience.
Reviews from plan members
"AR AG legal insurance has helped me so much – it’s taken all
the stress out of the process and has provided me with an
excellent lawyer. I am so happy I went with ARAG and I have
been recommending it to everyone I know that may benet
from their services."
– Nestor Los Angeles, CA
*A v e rage cost to employee without legal insurance is based on the average number of attorney hours for ARAG claims incurred in 2018 or 2019 and paid by December 31, 2020,
multiplied by $368 per hour. $368 is the average hourly rate for a U.S. attorney with 11 to 15 years experience according to "The Survey of Law Firm Economics: 2018 Edition."
Customer Care
When members need help or
just have a question regarding
their legal plan, they can call a
helpful and highly-trained, caring
Customer Care specialist who
will listen to their concerns and
oer suggestions for next ste
ps.
Maybe that’s why members rated
the service provided by ARAG
Customer Care a 9/10 in our 2020
ARAG Plan Member Satisfaction
Survey, or that it has been certied
as a Center of Excellence – one
of the most prestigious award
s
in the service and support
industry – for the 11th time.
$5$*OHJDOFRPP\LQIR
$FFHVV FRGH SFV
&DOO
43
Electronic Device Protection Program
(Optional – Participation is Voluntary)
En
rollment Information Claims Information
Employee Benefits Risk Management
mybenefits@pasco.k12.fl.us riskmanagement@pasco.k12.fl.us
(813) 794-2253 (813) 794-2520
Pasco County Schools (District) offer employees the
opportunity to purchase Electronic Device Protection
for their District assigned laptop or iPad. Participation is
optional, but
strongly
encouraged and
requires a single-
premium payment.
What is a single-premium payment?
• A one-time payroll premium deductio
n
• P
remiums are non-refundable
• Provides coverage for the January 1 –
D
ecember 31, plan year
• Coverage must be renewed each plan year
Device Single-Premium
Laptop $35.00
iPad $20.00
W
ho is eligible to purchase Electronic Device
Protection?
All District employees assigned a District owned laptop
or iPad are eligible to participate. The program is open
to new hires and current employees including
employees who are not eligible to participate in the
group health plan.
Who should consider purchasing Electronic Device
Protection?
• Employees who frequently travel with th
eir
l
aptop or iPad
• Employees who take their laptop or iPad home
on a regular basis
• Employees who often walk across campus with
their laptop or iPad
in hand
What
are the benefits of Electronic Device Protection?
The Electronic Device Protection Program provides
protection should your District assigned laptop or iPad
suffer any damage due to your negligence during the
coverage period. This protection relieves you of any
liability and subsequently no out of pocket cost
associated with the repairs or replacement.
Replacement Devices
If the District replaces an employee device during the
plan year, the employee has the option to purchase
new Electronic Device Protection to cover the new
device for the remainder of the plan year.
Stolen Devices
Reports of stolen devices must be substantiated by a
police report. The Electronic Device Protection plan will
become the secondary provider if other insurance is
present.
Examples of Covered Events:
• Accidental damage – includes cracked screens,
spilled liquids, fire/flood damage
•
Vandalism
• Power surge due to lightning
• Th
eft
Is there a deadline to enroll?
Yes. Current employees must enroll during the annual
open enrollment period. New employees must enroll
during their new hire benefit election period.
Employees not eligible to group health benefits must
email [email protected]
to enroll.
May
I purchase coverage for my personal electronic
devices?
Only work-related, District assigned devices are eligible
for coverage under the Electronic Device Protection
Program.
What is not covered?
The Electronic Device Protection Program does not
cover damages resulting from malicious intent,
vandalism or theft by the employee.
Are employees required to purchase coverage?
No. Participation in the program is strictly voluntary.
Employees who elect not to purchase Electronic Device
Protection may be responsible for any damage to the
device, consistent with Pasco County Schools’ Employee
Electronic Device Program and must return the device
and accessories to its original condition at time assigned
to employee.